Samples collected during this study will be processed at the research laboratory of St. Joseph’s Healthcare Hamilton using proprietary testing developed by St. Joe’s researchers.
McMaster HealthLabs (MHL), Air Canada, and the Greater Toronto Airports Authority (GTAA) have announced that they will partner on a voluntary COVID- 19 study of international travellers arriving at Toronto Pearson International Airport. The study’s core purpose is to gather information to explore the effectiveness of various quarantine periods for travellers. MHL is a non-profit organization that develops COVID-19 research initiatives and testing solutions to accelerate business recovery during the pandemic.
“MHL’s team of scientists and doctors from McMaster University, the Research Institute of St. Joe’s Hamilton, and other Canadian universities and research organizations, generates scientific COVID-19 data to keep Canadians safe and to support a strong economy,” said John Gilmour, MHL’s Chief Executive Officer. “Our study will provide data to help determine if an airport-based COVID-19 surveillance program is feasible, whether self-collection of COVID-19 testing is effective, and to explore options regarding the 14-day quarantine for international travel. The leadership of Air Canada and the GTAA in supporting COVID-19 research serves as a model for other organizations looking to make evidence-based decisions.”
“Air Canada has advocated for the adoption of rational, science-based measures in Canada relating to COVID-19, to allow for the prudent easing of travel restrictions and the mandatory 14- day quarantine, thereby striking a better balance for travellers and for the Canadian economy without adversely impacting public health. We are pleased to co-sponsor this extremely important study, which we believe should provide alternatives to the current blanket restrictions and quarantine,” said Dr. Jim Chung, Chief Medical Officer at Air Canada.
“Air Canada believes that issues arising from COVID-19 related to travel can be safely managed using a science-based approach. The study performed by MHL, whose team has years of infectious disease academic research experience, should improve the understanding of the prevalence of COVID-19 among travellers so that safety measures implemented are proportionate to the actual risk.”
Air Canada has been at the forefront of the airline industry in responding to COVID-19, including being among the first carriers globally to require customer face coverings onboard and the first airline in the Americas to take customers’ temperatures prior to boarding. In May it introduced a comprehensive program, Air Canada CleanCare+, to apply industry leading biosafety measures at each stage of the journey.
“The Greater Toronto Airports Authority is committed to a science-based approach that prioritizes the health and wellbeing of passengers and airport workers. That starts with the collection and analysis of data, led by McMaster HealthLabs through their travel study,” said Deborah Flint, President and CEO, GTAA. “We are pleased to partner with Air Canada in this critically important work and welcome the opportunity to work collaboratively with the Government of Canada on this and other initiatives to support the safe resumption of international travel.”
The month-long research project has been designed and will be conducted by MHL in accordance with research ethics board-approved scientific protocols. The study will be the largest of its kind and will seek to examine the number and percentage of arriving international travellers who test positive for COVID-19 during the federal government’s quarantine period. The findings of the study may be useful to the Government of Canada in its decision-making to control the spread of COVID-19 and in exploring policy options. Air Canada, as the largest Canadian airline operating out of Toronto’s Pearson International Airport, is providing resources and support for the study.
McMaster HealthLabs’ Scientific Director Dr. Marek Smieja, also a McMaster University professor and the study’s co-principal investigator, said: “MHL’s study will generate data to help us better understand and communicate the potential risk to the health of Canadians posed by international air travel and the risk of the importation of COVID-19.”
The molecular test for COVID-19 being used in this study was designed by Dr. David Bulir at the Research Institute of St. Joe’s Hamilton. This highly robust test has been deployed in multiple clinical and research labs across the province. Dr. Bulir serves as the Research Director of MHL and is a co-investigator of this study.
“Having scientific data to support decision-making about COVID-19 is critical to keeping Canadians safe as we work to get the economy moving,” said Dr. Vivek Goel, co-principal investigator of the MHL study, professor at the University of Toronto and a former CEO of Public Health Ontario.

Under the study:
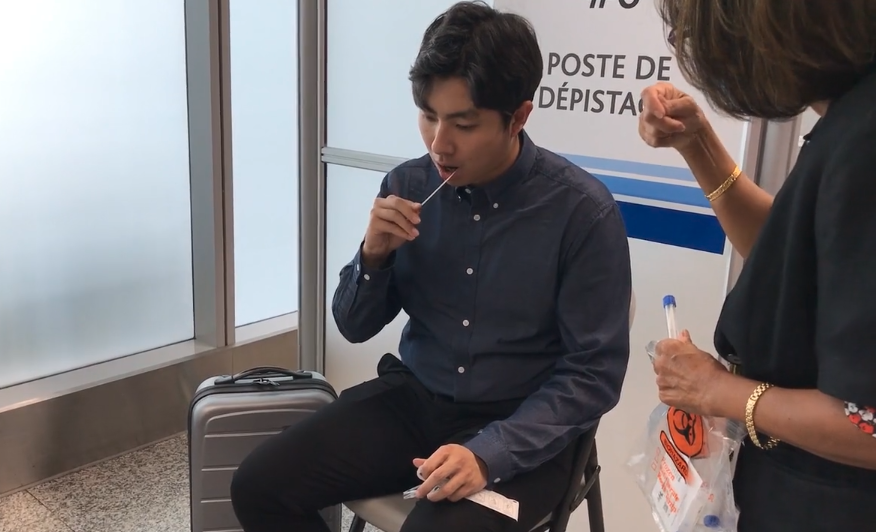
- Beginning Sept. 3, international travellers arriving at Toronto-Pearson Terminal 1 will be invited to take part in the study on a strictly voluntary basis after providing informed consent.
- Consenting participants will provide a sample to MHL researchers before leaving the airport and supply two additional samples that will be self-collected seven and fourteen days after arrival, coinciding with the federal government’s quarantine period.
- MHL will have samples analysed for COVID-19 at the Research Institute of St. Joe’s Hamilton using polymerase chain reaction (PCR) testing.
- Participants will be notified electronically of the first results within a couple days. Data collected will remain confidential and will be anonymously aggregated for the purpose of the study.
- An independent data analysis will be conducted at the Dalla Lana School of Public Health at the University of Toronto under the supervision of the Principal Investigators who will have responsibility for publishing the results in peer reviewed journals and for supporting MHL in broadly sharing the study’s findings.
About McMaster HealthLabs:
McMaster HealthLabs (MHL) is a non-profit organization that develops COVID-19 research initiatives and testing solutions to keep Canadians safe and to get them back to work. MHL works with a team of scientists and doctors from McMaster University, the Research Institute of St. Joe’s Hamilton in Ontario, and other Canadian universities and research organizations. MHL partners with Verto Health, leveraging its innovative digital twin technology solutions in MHL research initiatives. MHL is collaborating with Deloitte Canada for strategic and operational advisory support on this study. MHL is focused on curbing the human, economic and social costs of COVID-19 by creating scientific research initiatives that help Canadian leaders make evidence- based decisions.
Services available to cleaners, administrators as well as nurses and doctors
Dan Taekema · CBC News · May 06, 2020

Randi McCabe is a clinical psychologist at St. Joseph’s Healthcare Hamilton who helped design mental health services for health and community-care workers.
St. Joseph’s Healthcare Hamilton has a message for anyone working on the front line of the COVID-19 pandemic: “You don’t have to suffer alone.”
The hospital system is stepping up as the regional lead for mental health support, covering the city and everything west of it and offering those dealing directly with the pandemic — in any setting or role —someone to talk to.
“We’re really talking about anybody who’s on that front line. It could be housekeeping staff … nutrition staff, admin staff checking people in at the door,” said Randi McCabe, a clinical psychologist at St. Joe’s. “It could be people working in shelters or hospice.”
McCabe’s family knows how stressful and scary the virus can be. Her husband works on a COVID-19 unit and whenever he comes home he makes sure to wash his clothes and shower before speaking with his loved ones, she said.
The possibility of passing along the virus is a source of anxiety others who have continued to work through the pandemic also share.
“There’s a big fear of contaminating their family,” explained McCabe. “The stress of ‘Well how do I keep myself separate from my family? Am I cleaning myself enough?'”
Concerns about people’s own health and safety as well as exhaustion from working in a setting, such as a long-term care home, that doesn’t have enough staff also create a “huge burden of stress,” she said.
Then there’s the weight of trying to treat someone with the virus only to watch them die.
“It’s very painful emotionally to be involved when someone actually passes away from COVID,” said McCabe. “It’s very sad.”
The province announced Tuesday it was expanding virtual mental health services.
“In order to help stop the spread of this deadly virus our frontline workers are working long hours in stressful situations and people across the province are doing their part by staying home, in many cases alone,” stated Health Minister Christine Elliott in a media release.
“We know these actions are not easy and can cause stress, anxiety and other mental health issues. That’s why we are providing virtual mental health supports, allowing people to get the help they need while still physically distancing.”
St. Joe’s has partnered with the Canadian Mental Health Association to determine what support is best for each individual who calls in or fills out an online intake form.
Services include self-help, counselling by phone or online, peer-to-peer support and in-person visits for those in crisis.
Anyone who’s finding their sleep, appetite or relationships with loved ones affected by the stress of their role is encouraged to reach out.
The pandemic has introduced a “new abnormal,” said McCabe, and chances are it will last until a vaccine can be found. That means the stress will be sticking around too.
“This isn’t going anywhere and it’s actually going to change how we do things for quite a ways to come,” she added.
“There is help and hopefully some relief for people if they’re suffering from the effects of their stressful positions right now.”
· CBC News ·
A team of international experts, including medical specialists from Hamilton and Toronto universities and research institutes has produced guidelines on how to care for COVID-19 patients in intensive care.
The team managed to put the guidelines together in less than three weeks, instead of following the typical process that takes as long as a year.
The process was rushed as the number of COVID-19 cases, critically ill patients and deaths continue to climb around the world.
In Ontario alone, CBC discovered that the number of patients in critical care beds exceeded 430 as of Monday. Of these, 125 are confirmed to have the virus while the remaining 353 are “suspected” cases.
The team includes six experts from McMaster University in Hamilton, and has members from University of Toronto, Sunnybrook Health Sciences Centre, St Joseph’s Healthcare’s GUIDE research methods group in Hamilton and the Population Health Research Institute, also in Hamilton.
The recommendations released by the Surviving Sepsis Campaign COVID-19 panel hopes to better guide frontline workers as they tackle the increasing demand within the intensive care unit (ICU).
The 54 guidelines suggest the best infection control, care measures and therapy practices.
Of the recommendations, four are best practice statements, nine are strong and 35 are weak. The top four include the wearing of personal protective equipment during invasive procedures, the use of negative pressure rooms, intubation by airway management experts and closely monitoring adults in critical condition.
“Previously there was limited guidance on acute management of critically ill patients with COVID-19, although the World Health Organization and the United States Centers for Disease Control and Prevention have issued preliminary guidance on infection control, screening and diagnosis in the general population,” said sepsis panel member Waleed Alhazzani in a press release.
Alhazzani is also an intensive care physician at St. Joseph’s Healthcare Hamilton.
To compile this list, the experts started out by proposing 53 questions they felt were relevant to managing COVID-19 in the ICU.
Individually they searched academic literature and took note of information that answered their questions. This evidence was then assessed using reliable clinical practice standards, with robust practices making it to the final cut.
The full set of guidelines were co-published online Friday in the Critical Care Medicine and Intensive Care Medicine journals.
The Brantford Expositor
By: Susan Gamble
News: March 20, 2020
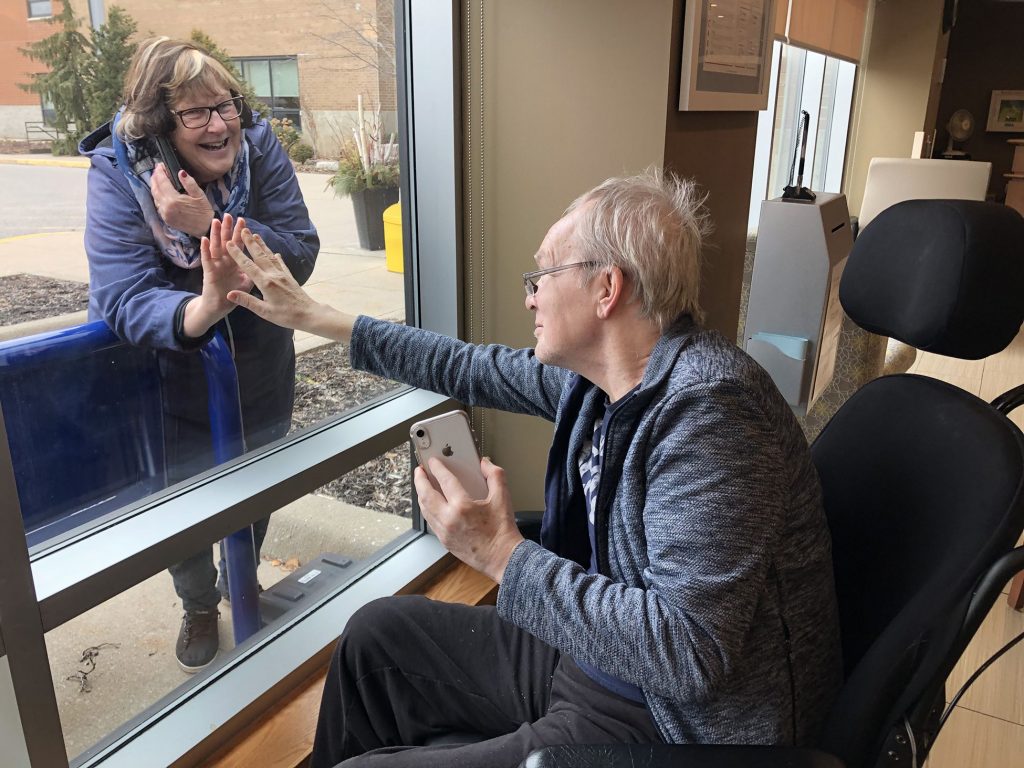
Bill Johnston reaches out to connect to his wife Betty through the window at St. Joseph’s Lifecare Centre where recreational therapists have made an area available for seniors to see and chat by phone with their families. Johnston owned and operated the Burford Times for 30 years.
While COVID-19 is wreaking havoc on visits and work schedules at area nursing homes, St. Joseph’s Lifecare is working to ensure both patients and visitors feel supported.
“There’s been a lot of creativity being used,” said David Wormald, president of the Lifecare Centre which is now restricting visitors in almost all cases.
“It’s heartbreaking to have this lock-down in place but we know it’s in the best interests of our residents, staff and those in the community. So, meanwhile, our staff is working to engage with residents and family to connect them.”
Nancy Billard, who handles communications for the facility, said window visits are just part of ‘Project Feel Good’, implemented to help support staff and residents through the pandemic.
“We can’t give hugs but we’re saying however you can make someone feel good in lieu of that – a smile, thumbs up, wave or positive comment – will help.”
Billard said there was some unease among the residents over the first few days of changes but a “feeling of calmness” has settled on the building and is making it’s way from staff to the seniors.
“We’ve maintained 100 percent staffing levels since this started and people have even returned from stay-at-home vacations to help out. It’s been amazing and I have to retreat to my office and get my tissues out two or three times a day.”
Along with scheduling time and providing a phone at the ground-floor window, staff is also working to arrange Skype, Facetime or video-conferencing for the families.
And, all the positive comments that pour in on the St. Joseph’s Facebook page are being printed out as posters and hung around the facility so workers can see how much they are appreciated.
The appreciation flows both ways: Billard said John Ansell from The Keg Steakhouse and Bar donated multiple cases of fresh produce to the Stedman Hospice adjacent to the Lifecare Centre this week as the restaurant closed its doors Tuesday.
“We are incredibly thankful to have received this generous gift,” Billard said, adding that anything the hospice couldn’t use went to the Brantford Food Bank which is experiencing a higher demand for help.
“Our staff is certainly finding it difficult but people are really coming together,” said Wormald.
“I am immensely proud of and applaud the compassionate care and courage of our staff and physicians. They mobilized to support each other and keep our residents and community safe.”