Samples collected during this study will be processed at the research laboratory of St. Joseph’s Healthcare Hamilton using proprietary testing developed by St. Joe’s researchers.
McMaster HealthLabs (MHL), Air Canada, and the Greater Toronto Airports Authority (GTAA) have announced that they will partner on a voluntary COVID- 19 study of international travellers arriving at Toronto Pearson International Airport. The study’s core purpose is to gather information to explore the effectiveness of various quarantine periods for travellers. MHL is a non-profit organization that develops COVID-19 research initiatives and testing solutions to accelerate business recovery during the pandemic.
“MHL’s team of scientists and doctors from McMaster University, the Research Institute of St. Joe’s Hamilton, and other Canadian universities and research organizations, generates scientific COVID-19 data to keep Canadians safe and to support a strong economy,” said John Gilmour, MHL’s Chief Executive Officer. “Our study will provide data to help determine if an airport-based COVID-19 surveillance program is feasible, whether self-collection of COVID-19 testing is effective, and to explore options regarding the 14-day quarantine for international travel. The leadership of Air Canada and the GTAA in supporting COVID-19 research serves as a model for other organizations looking to make evidence-based decisions.”
“Air Canada has advocated for the adoption of rational, science-based measures in Canada relating to COVID-19, to allow for the prudent easing of travel restrictions and the mandatory 14- day quarantine, thereby striking a better balance for travellers and for the Canadian economy without adversely impacting public health. We are pleased to co-sponsor this extremely important study, which we believe should provide alternatives to the current blanket restrictions and quarantine,” said Dr. Jim Chung, Chief Medical Officer at Air Canada.
“Air Canada believes that issues arising from COVID-19 related to travel can be safely managed using a science-based approach. The study performed by MHL, whose team has years of infectious disease academic research experience, should improve the understanding of the prevalence of COVID-19 among travellers so that safety measures implemented are proportionate to the actual risk.”
Air Canada has been at the forefront of the airline industry in responding to COVID-19, including being among the first carriers globally to require customer face coverings onboard and the first airline in the Americas to take customers’ temperatures prior to boarding. In May it introduced a comprehensive program, Air Canada CleanCare+, to apply industry leading biosafety measures at each stage of the journey.
“The Greater Toronto Airports Authority is committed to a science-based approach that prioritizes the health and wellbeing of passengers and airport workers. That starts with the collection and analysis of data, led by McMaster HealthLabs through their travel study,” said Deborah Flint, President and CEO, GTAA. “We are pleased to partner with Air Canada in this critically important work and welcome the opportunity to work collaboratively with the Government of Canada on this and other initiatives to support the safe resumption of international travel.”
The month-long research project has been designed and will be conducted by MHL in accordance with research ethics board-approved scientific protocols. The study will be the largest of its kind and will seek to examine the number and percentage of arriving international travellers who test positive for COVID-19 during the federal government’s quarantine period. The findings of the study may be useful to the Government of Canada in its decision-making to control the spread of COVID-19 and in exploring policy options. Air Canada, as the largest Canadian airline operating out of Toronto’s Pearson International Airport, is providing resources and support for the study.
McMaster HealthLabs’ Scientific Director Dr. Marek Smieja, also a McMaster University professor and the study’s co-principal investigator, said: “MHL’s study will generate data to help us better understand and communicate the potential risk to the health of Canadians posed by international air travel and the risk of the importation of COVID-19.”
The molecular test for COVID-19 being used in this study was designed by Dr. David Bulir at the Research Institute of St. Joe’s Hamilton. This highly robust test has been deployed in multiple clinical and research labs across the province. Dr. Bulir serves as the Research Director of MHL and is a co-investigator of this study.
“Having scientific data to support decision-making about COVID-19 is critical to keeping Canadians safe as we work to get the economy moving,” said Dr. Vivek Goel, co-principal investigator of the MHL study, professor at the University of Toronto and a former CEO of Public Health Ontario.

Under the study:
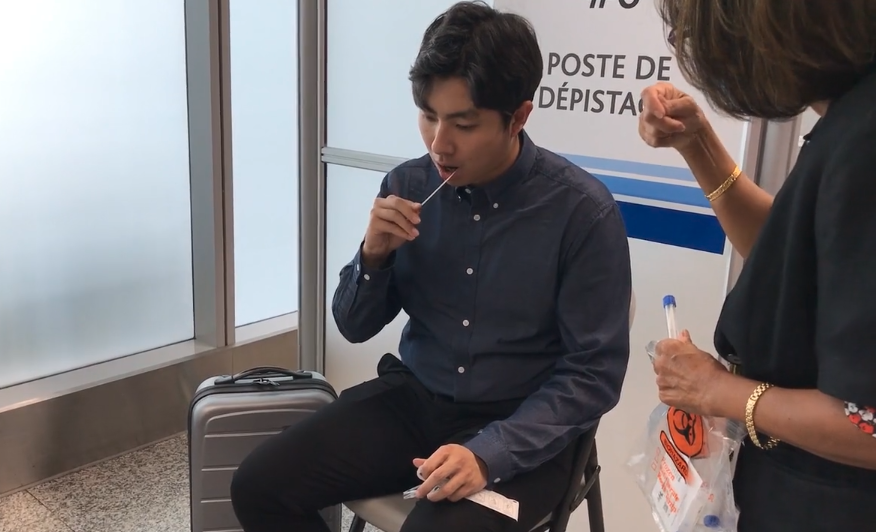
- Beginning Sept. 3, international travellers arriving at Toronto-Pearson Terminal 1 will be invited to take part in the study on a strictly voluntary basis after providing informed consent.
- Consenting participants will provide a sample to MHL researchers before leaving the airport and supply two additional samples that will be self-collected seven and fourteen days after arrival, coinciding with the federal government’s quarantine period.
- MHL will have samples analysed for COVID-19 at the Research Institute of St. Joe’s Hamilton using polymerase chain reaction (PCR) testing.
- Participants will be notified electronically of the first results within a couple days. Data collected will remain confidential and will be anonymously aggregated for the purpose of the study.
- An independent data analysis will be conducted at the Dalla Lana School of Public Health at the University of Toronto under the supervision of the Principal Investigators who will have responsibility for publishing the results in peer reviewed journals and for supporting MHL in broadly sharing the study’s findings.
About McMaster HealthLabs:
McMaster HealthLabs (MHL) is a non-profit organization that develops COVID-19 research initiatives and testing solutions to keep Canadians safe and to get them back to work. MHL works with a team of scientists and doctors from McMaster University, the Research Institute of St. Joe’s Hamilton in Ontario, and other Canadian universities and research organizations. MHL partners with Verto Health, leveraging its innovative digital twin technology solutions in MHL research initiatives. MHL is collaborating with Deloitte Canada for strategic and operational advisory support on this study. MHL is focused on curbing the human, economic and social costs of COVID-19 by creating scientific research initiatives that help Canadian leaders make evidence- based decisions.
St. Joseph’s Health System & Niagara Health launch new pilot surveillance project to protect the most vulnerable in our health system
April 20, 2020 – COVID-19 has had a devasting effect within many congregate care facilities caring for vulnerable elderly residents, prompting the Ontario government to call for greater testing in long-term care and retirement homes.
With that in mind, St. Joseph’s Health System (SJHS) and Niagara Health are taking the vital step in testing all asymptomatic patients, residents and select staff within its long-term care, retirement home and congregate settings as part of a pilot surveillance project.
Under the directive of Dr. Tom Stewart, CEO of St. Joseph’s Health System and Niagara Health, and the SJHS Executive team, supported by Research Institute and Lab, the project will test our most vulnerable patients and residents, including those living in long-term care, to save lives.
Researchers at the Research Institute of St. Joe’s Hamilton, McMaster University, Guelph Assessment Centre, Public Health Ontario Lab and select public health units across the GTA are working together to test thousands of samples collected from long-term care facilities and retirement homes.
“We are testing the prevalence of asymptomatic COVID positive cases that could inform future testing strategies and prevention measures to curb the spread of this devastating virus and save lives,” Says Dr. Jack Gauldie, Vice-President of Research at St. Joseph’s Healthcare Hamilton. “It’s vital we learn how we can protect our most vulnerable population and our staff today and, in the future. We need to share our findings widely to make changes to how we protect the elderly living in congregate settings.”
“St. Joseph’s Health System and Niagara Health are committed to delivering integrated care across the continuum,” says Dr. Tom Stewart. “With our capacity and network of hospitals, research laboratories, long-term care home, Home Care, and retirement homes, it would be irresponsible not to put our collective efforts together in the fight against COVID-19. If our surveillance project demonstrates that asymptomatic cases can be COVID positive, it will dramatically change the COVID-19 response and prevention strategy going forward and most importantly will save lives.”
Testing of staff, residents and patients across St. Joseph’s Health System and Niagara Health has already begun.
“We have tested all 111 long-term care residents for COVID-19 whether they had symptoms or not. All results have come back negative,” Says Lynn Guerriero, President of Niagara Health. “We need to do everything we can to minimize the risk to our residents, and testing will continue on a regular basis to support a safe environment and understand more about this virus.”
The Office of the Chief Medical Officer of Health, working with the Ministry of Long-Term Care and Ontario Health, will review results from these tests and work to refine testing guidance as appropriate to support continued testing of asymptomatic residents and staff.
Partnering Organizations
- Research at St. Joes
- St. Joseph’s Villa Dundas
- St. Joseph’s Health Centre Guelph
- St. Joseph’s Lifecare Centre Brantford & Stedman Community Hospice
- St. Joseph’s Home Care
- Niagara Health
- Hamilton Regional Laboratory Medicine Program
- McMaster University
- Wellington-Dufferin-Guelph Public Health
- Guelph Assessment Centre
- Hamilton Public Health
- Brant County Health Unit
- Niagara Regional Public Health
- PHO Lab
- Ontario Public Health
- Ministry of Health & Ministry of Long-Term Care
BY DON MITCHELL GLOBAL NEWS
Two well-known philanthropists are set to give Hamilton health researchers a $3.3-million boost to help fund urgent research projects connected to the COVID-19 pandemic and mental health.
In a letter to the community, Charles and Margaret Juravinski say they are donating funds to free everyone from the “terrible virus,” and allow the public to “live and move about without fear of spreading or picking it up.”
“Like everyone, we are deeply troubled by the fearsome threat of COVID-19, which has truly changed the world in just a few months,” the couple said in their letter.
“We are concerned not for ourselves, but for the people around us: our friends and family, our neighbours near and far, the people who work in our community’s grocery stores, restaurants and hospitals and the kids who should be out playing in our schoolyards.”
The money is an advance on a pledge made in May when the couple promised to divide their $100-million estate between Hamilton Health Sciences, McMaster University and St. Joseph’s Healthcare Hamilton, a gift they say would generate up to $5 million annually for the three agencies under the banner of the Juravinski Research Institute.
Charles, 90, and Margaret, 88, known for endowments with a number of projects connected to the city, McMaster University, and healthcare, compare the COVID-19 pandemic to a number of “frightening problems” they experienced during their lifetime including the Great Depression, the Second World War and the scourge of polio.
“Our wish is that it may inspire hope,” the couple said of the donation, “We hope it will produce results that benefit people immediately. We urge others to find ways to give what they can.”
In a joint statement, Hamilton Health Sciences, McMaster University and St. Joseph’s Healthcare Hamilton say the funding will support eight collaborative research projects which include:
- A study on the effectiveness of N95 respirators or medical masks
- A three-part study on the impact of the pandemic on hospital emergency departments and staff
- speed up of diagnostic testing protocols for viral pathogens responsible for the COVID-19 using robotics
- An age-related study of 50,000 people ages 45 to 85 to close in on factors that appear to protect against or increase the risk of developing symptoms connected to COVID-19
- COVID-19 repository for storing human biological samples
The money is also earmarked for three mental health projects including a study on the impact of substance use in relation to the brain development of young adults, technology to identify brain anomalies following a mild traumatic brain injury, and AI technologies offering data on potential treatments to aid youth mental health.
Hamilton Spectator
July 18/19 by Joanna Frketich

Hamilton Health Team Co-Chairs John Fleming and Bernice King
Hamilton and Burlington organizations want to be among the first to adopt a major overhaul of the health care system by the Progressive Conservative government.
Health and social service agencies have banded together in each city to put forth separate applications to create Ontario Health Teams (OHT), which are expected to oversee dramatic changes in how local care is provided.
Both proposals got the go-ahead Thursday to move to the next stage in the application process to form the first OHTs in the province.
“I don’t think anybody at the table is sitting there because they think the whole thing is broken,” said Paul Johnson, who is representing the city in Hamilton’s proposed health team. “They are sitting at the table because they see such opportunity.”
The legislation for the health system revamp came into effect June 6 under the Connecting Care Act. An investigative series Operation Health Care Reform by The St. Catharines Standard and The Hamilton Spectator starting Saturday (July 20) will provide the most comprehensive coverage to date of the overhaul considered the biggest change since Medicare.
The plan announced in February puts a super agency named Ontario Health in charge of the entire health care system — from hospitals to community care to organ donation to cancer care. The super agency will oversee dozens of regional teams made up primarily of health and social service organizations working together to integrate services locally and help area residents navigate the system.
The Ministry of Health got over 150 OHT applications in May provincewide despite few details being known about how the teams will be governed, funded or operate. The province has said, OHTs will evolve over time based on the experiences of the initial groups.
“This could be the biggest transformation we’ve seen certainly in a long time,” said Johnson. “If we work differently, we can really change the outcomes in terms of better care.”
The Hamilton application is made up of 18 health and social services agencies including Hamilton Health Sciences, St. Joseph’s Healthcare, McMaster University and the city. But there is room for more to join.
“Our principle really is there is an open chair,” said Johnson. “I don’t think any of us are convinced the table is full.”
What makes the Hamilton bid particularly unique is that it is chaired by former cancer patients John Fleming and Bernice King.
“I haven’t been part of too many processes where we really have embedded a patient experience right from the beginning,” said Johnson. “Normally we would get through these first applications and say, ‘You know we really need to find some patients.’ Of course, we’ve decided what we’re doing long before.”
For Hamilton’s OHT application, patients are at the forefront of mapping out a new local health care system.
“It was an opportunity I couldn’t pass up,” said King, who was treated for lung and gynecological cancer.
Both King and Fleming feel this is a chance to give back to the system that helped them when they needed it most and improve it for the next patients.
“I’m here partly because this city and all of its health care systems saved my life literally,” said Fleming who was treated for melanoma. “I’m 100 per cent on board with what is going on and I want to contribute and I want to help.”
He describes their job as being “the relentless conscience of this project to never lose sight of keeping patients at the centre of this.”
The Burlington group also put patients first when it decided to make family medicine the focus of its application with all but two of the eight organizations being primary care providers.
“Our team recognizes the importance of primary care as the foundation of the health care system and that’s why I agreed to sign up for it,” said family physician Dr. Harpal Singh, who is the co-chair of the proposed Burlington OHT. “We feel this kind of model really should be the model of care throughout Ontario.”
So far the proposed Burlington team accounts for 60,000 rostered patients but it’s also hoping to grow.
“We’re still trying to get the word out to physicians in Burlington,” said Singh, lead doctor at the North Burlington Medical Centre Family Health Group. “Due to privacy laws we’re not even allowed to have access to physicians’ emails without their permission. These are the kinds of barriers that inhibit care for patients.”
Teams being considered to form the first OHTs have been asked to put in a full application to represent a geographic area with a population up to 500,000. The early adopters will be announced in the fall.
Both Hamilton and Burlington groups are confident they will be among the first OHTs because health and social service organizations have long collaborated in this area.
“Why I think we’re a bit optimistic is that we’ve put the work in prior to this,” said Johnson. “This really builds on work that’s been going on in Hamilton. We’ve been thinking about what health care means in the broadest sense of that term from the social determinants of health umbrella.”
One of the reasons Hamilton is so far ahead is an ongoing project started in 2010 by The Spectator called Code Red that found glaring disparities between neighbourhoods in Hamilton including a 21-year difference in average age at death. It long ago helped foster ongoing collaboration between health and social service agencies.
Johnson gives the example of the patient with chronic obstructive pulmonary disease who ends up in the emergency room four to five times every summer because the progressive lung disease is exacerbated by heat.
“This primary care physician is saying it would be great if they had an air conditioner and I say we have a program that could deliver an air conditioner,” said Johnson. “Those are the little things.”
The OHTs will aim to bridge the gaps that often leave patients lost by having multiple providers band together to take joint accountability for the entire journey through the system.
“I often look around and think we have it all here,” said Johnson. “What is holding us back is the inability to do the things we know we need to do. Sometimes that is because we don’t have the relationships with each other to even know someone else could do it. We’re a bit discoordinated.”
Drastically changing how health care providers interact is the only way the system will be able to cope with the growing and aging population, says Singh.
“Healthcare often is relatively insatiable in the amount of expectations that we have,” said Singh. “In order to work with limited resources we need to organize ourselves better.”
Joining the OHT requires a leap of faith considering neither group has come up with a governance structure yet or knows what will happen to their funding when the province provides one envelope of cash per patient to be shared among all the services.
“We’d be naïve to say everybody around the table is not thinking about that,” said Johnson. “When people already have a bit of a relationship — believe me it’s not all kumbaya moments — there is at least that level of trust that we are going to continue to work at this and even if it’s not perfect yet we’ll keep making it better.”
There’s no startup funds so the organizations involved have to find a way to pay for the costs of the application and the administration of the proposed OHT.
“There is no pot of money being offered by Queen’s Park,” said Fleming. “It’s figure out how to put this together within the resources of our team.”
In addition, the OHT has to navigate making sure small organizations in the group get a voice when massive players like HHS, St. Joseph’s and Joseph Brant Hospital are involved.
“There are physicians in Burlington who have felt that the hospital has their agenda and family doctors have their agenda and they don’t necessarily align,” said Singh. “We work in that fragmented and siloed way and it becomes really increasingly difficult for patients to get proper care or to negotiate through that system.”
Both groups say they won’t quit even if they aren’t chosen to be among the first teams.
“Whether we are an early adopter or not, our position has been that we are going ahead at the same pace that we have been to date, this is such important work.” said Dr. Cheryl Williams, co-chair of the proposed Burlington OHT and executive vice president clinical at Joseph Brant.
Her co-chair Singh expects the province to keep working with teams not initially chosen until they are ready to become an OHT in future waves of the roll out.
“Our plan to co-operate, break down barriers and provide the best kind of care for our patients is going to move forward,” he said. “It’s just going to get stronger.”
Two Hamilton researchers will study post traumatic stress in emergency services
Media Outlet: Hamilton Spectator | Date: February 14, 2019 | Reporter: Joanna Frketich
Hamilton researchers are teaming up with scientists in France to determine the links between mind and body that could one day bring about more personalized mental health treatments.
“The hope for the patients one day is that when they come with depression, we don’t give them only an anti-depressant,” said Dr. Flávio Kapczinski, professor of psychiatry at McMaster University and St. Joseph’s Healthcare.
“We give them a whole strategy on how they would get outside the risk zone for depression.
“We could give them exercise, correct their metabolism with some sort of diet and give them anti-inflammatories.”
The partnership with the Pasteur Institute was one of three new Hamilton mental health projects launched in February.
The other two will investigate post-traumatic stress injuries (PTSI) in public safety personal such as firefighters, paramedics, police officers and correctional workers.
Both received grants of up to $150,000 from the Canadian Institutes of Health Research as part of $2.95 million in federal funding announced Feb. 8 to studies that increase understanding of how to identify, treat and prevent PTSI.
Margaret McKinnon, chair in mental health and trauma at McMaster, will do a randomized control trial to test a new way to treat PTSI in public safety personal with other health conditions.
Occupational therapist Sandra Moll plans to design a mobile health approach to prevention and peer support.
“Public safety personnel put themselves in harm’s way to protect Canadians, putting them disproportionately at risk of post-traumatic stress injuries,” federal minister of public safety and emergency preparedness Ralph Goodale said in a statement.
“Our country must do more to protect the mental well-being of public safety officers on-the-job. The initiatives will help address gaps in PTSI research and inform long-term plans to support the mental health and well-being of our public safety personnel.”
Meanwhile, the new partnership with the French researchers is significant because it gives St. Joseph’s Healthcare and McMaster access to basic science research that they don’t have now.
In turn, they offer Pasteur large cohorts of patients from West 5th hospital that the French are currently missing.
“We are accumulating a lot of data in this field now and thanks to this collaboration we’re going to have access to large cohorts,” head of Pasteur’s perception and memory unit Dr. Pierre-Marie Lledo said during a trip to Hamilton on Feb 7.
“We get a full picture of how the brain functions by having access to the clinical data.”
It’s also unique because French researchers generally team up with Quebec investigators.
“When France would partner with Canada they never crossed the Gatineau River,” said Kapczinski.
“Now the commitment of the French Embassy is to bring to the attention of French scientists this whole perspective of dealing with many other centres like McMaster. We are looking to the idea of strengthening the scientific links between Canada and France.”
So far, funding is primarily from their own institutions and the French Embassy, but they are working on applying for grants to study many different potential mind and body links.
“We were finding our patients when they have depression, they have a lot of inflammation in their blood,” said Kapczinski.
“We didn’t know the cause of that. Pasteur is famous because it’s where immunology and inflammation started to be understood … so we reached out to the director and he was very excited.”
Other questions vary from gut bacteria to exercise to metabolism to electric signalling between fatty tissues of the brain.
“People who suffer from depression they suffer a lot of brain changes like accelerated aging,” said Kapczinski.
“The brain and the body as a whole starts to age faster and we want to understand the mechanisms associated with that.”

