
(HAMILTON, NIAGARA) – NOVEMBER 12, 2020 – COVID Care @ Home is a new model of care delivered by St. Joseph’s Home Care (SJHC), in partnership with St. Joseph’s Health System (SJHS), Niagara Health and community partners that connects patients to care wherever they are, whenever they need it.
Starting at St. Joseph’s Healthcare Hamilton and Niagara Health, with rapid expansion to Kitchener, this new model of care for COVID patients will provide 24/7 access to high-quality care from one integrated team in the home and in community settings like retirement homes, shelters and hospices.
COVID Care @ Home is a uniquely designed program intended for those with a confirmed COVID diagnosis who do not require hospitalization. Complimenting existing local COVID initiatives, the program will support integrated care at home, early discharge from hospitals with supports and help to prevent hospitalization. It will also help to prevent outbreaks by providing Infection Prevention and Control (IPAC) and coaching support for community congregate settings.
Patients will be assessed to determine what level of service will be provided. Vulnerable patients who are at risk of hospitalization and who require additional supports and services will have access to an integrated clinical care team, remote monitoring and at-home and virtual visits to support a safe recovery at home. This same model of care will be available to patients discharged from hospital so they can safely return home sooner.
This innovative, flexible model would provide COVID patients access to services that may not typically be within the scope of traditional home and community care supports. Patients will be cared for by one integrated team representing a variety of providers whose clinical decisions are empowered through the use of a single electronic patient record to support patients in the following ways:
- Virtual Care (phone, video and remote patient monitoring)
- One number to call 24/7
- One clinical team
- One electronic record
- System navigation / connection to social supports
- Access to specialists
- IPAC Support
St. Joseph’s Home Care will lead this innovative transformation to connect home care to a broad range of services for COVID patients and work in collaboration with other service provider organizations and primary care.
SJHS is one of the largest healthcare organizations in Canada, and the only system in Ontario delivering a full continuum of integrated health care services.
“We’ve learned a tremendous amount about COVID-19 over the last several months,” said Tom Stewart, St. Joseph’s Health System President and CEO and CEO of Niagara Health. “This new program builds on partnerships and learnings by increasing our focus on virtual care and specialized COVID care teams that crosses normal silos of care. This will help us through the second and future waves of the pandemic as well as prepare us for system transformation needed in healthcare.”
The program is designed to support older adults who are at greater risk of physical and mental health decline. Patients will be enrolled by the clinical teams at the time of their COVID 19 diagnosis.
The new model will also help to protect capacity in hospitals by expanding supports and services in the community through a dedicated team that will facilitate care at home, support safe discharges from hospital and limit unnecessary Emergency Department visits. This will help hospitals to maintain capacity and services during a second wave as well as continuing scheduled surgeries to reduce wait lists and backlogs.
About St. Joseph’s Home Care
Since 1921, St. Joseph’s Home Care has provided high quality, values-based home and community services in a spirit of compassion and dedication. We have evolved from a nursing agency to offering a much broader range of services, and our steadfast commitment to delivering exemplary client-focused care to the Hamilton community continues.
About St. Joseph’s Health System
St. Joseph’s Health System (SJHS) is one of the largest healthcare organizations in Canada, and is the only system in Ontario delivering a full continuum of health care services. SJHS is a globally recognized leader for innovation in models of patient-centred integrated care. SJHS has a unique partnership with Niagara Health to leverage each organization’s strengths to bring better care to the people in the communities we serve.
About Niagara Health:
Niagara Health is a regional healthcare provider with multiple sites and a growing network of virtual and community-based services. We provide a wide range of inpatient and outpatient services to more than 450,000 residents across Niagara, including Acute Care, Cancer Care, Cardiac Care, Complex Care, Emergency and Urgent Care, Kidney Care, Long-Term Care, Mental Health and Addictions, Stroke Care and Surgical Care.
About St. Joseph’s Healthcare Hamilton
As a premier academic and research healthcare organization, St. Joseph’s Healthcare Hamilton is committed to making a difference in people’s lives and creating a lasting future for our community through integrated health services and internationally recognized programs. Our threefold mission is to provide dynamic research, revolutionary methods in health sciences education and the highest standard of clinical care in a spirit of compassion, innovation and commitment.
For More Information:
Patrick Moore
Senior Public Affairs Specialist, St. Joseph’s Health System
M: 905.870.1293 | E: pmoore@stjoes.ca
Steven Gallagher
Communications Specialist, Niagara Health
P: 289-696-6767 | E: Steven.Gallagher@niagarahealth.on.ca
Susan Gamble, The Brantford Expositor
Published on: May 4, 2020
The physical distancing requirements aimed at stopping the spread of COVID-19 have meant changes in how people can say goodbye to their loved ones at the Stedman Community Hospice,
“Our rules have changed but our overall objective is still the same – to ensure the best possible hospice experience for the patient, family and their visitors,” said executive director Elaine Calvert.
She said patients and their family members understand the new guidelines before admission.
“Everyone is provided with the information prior to an admission decision so they can understand the rules before they come. We make sure there’s a full awareness.”
The biggest change is that the hospice, with few exceptions, permits only one designated family member to be with a patient during the admission phase and one family member at a time when death is imminent. It’s similar to rules at Brantford General Hospital, where visitors are barred except for specific compassionate grounds to see dying patients.
But the design of the hospice’s Hankinson House, which opened in 2014, makes it accessible for “window visits,” said Calvert. Each of the 10 rooms that house patients has a large low window.
“They’re very popular and we are so fortunate to have a building that can accommodate privacy.”
A large deck soon will accommodate outdoors visits, too.
Hankinson House also is outfitted with technology that allows people to visit using FaceTime and Skype. And staff is on hand to support phone calls and virtual visits.
“We’re seeing every kind of device and all kinds of virtual presence you can imagine,” Calvert said. “Sometimes it even means combining a phone call with a window visit.”
Such visits are planned and co-ordinated with the staff.
“We’ve had to get very creative,” said Calvert.
“These are such unusual times but I could not be more proud of our staff. The level of co-ordination and commitment they demonstrate each day to ensure the patients and their families are supported is amazing.”
All visitors to the hospice are screened and staff wear masks and follow physical distancing guidelines set by the province.
Calvert said the hospice misses its volunteers who helped in the kitchen and with maintaining gardens.
“They are such an important part of the team and we very much look forward to welcoming them back.”
Despite the new rules, no one has turned down admission to Hankinson House, said David Wormald, president of the St. Joseph’s Lifecare Centre, which runs the hospice, along with the adjacent long-term care residence..
There have been no confirmed cases of COVID-19 in residents of either the hospice or at long-term residence.
A COVID-19 outbreak was declared at St. Joseph’s on April 2 after a staff member at the long-term residence tested positive for the virus. That outbreak was declared over on April 12 but a second staff member tested positive April 23. But subsequent extensive testing has yielded no further positive results.
“We took a very proactive approach early on and our staff is absolutely dedicated to our hospice and long-term residents,” said Wormald. “They’re showing such commitment and living our mission of compassion, courage and care.”
He said St. Joseph’s considers it essential to protect its staff, residents and their family members.
“These are quite extraordinary times but we continue to be vigilant.”
Sunday was to be date for the 16th annual Hike for Hospice, which has been postponed due to the virus. The hospice has an annual operating budget of about $3 million, with about half funded by community donations through the St. Joseph’s Lifecare Foundation. Last year’s hike brought in just over $338,000.
The hike was also meant to mark the official retirement of Olga Consorti from the president and CEO role she has held with the foundation for the past 30 years. She has agreed to stay in the role until at least the end of June.
SGamble@postmedia.com
@EXPSGamble
A beautiful prayer and message of hope from Sister Anne Anderson, Chair, Board of Directors, St. Joseph’s Health System, during this difficult time.
Representatives from healthcare organizations across the province gathered on January 23, 2020, to learn about St. Joseph’s Health System (SJHS)’s Integrated Comprehensive Care (ICC) program and how evidence-based models of Integrated Care could be applied in their organizations to support their Ontario Health Teams. The event is the first in a series of educational seminars, called Integrated Care Discovery Sessions, that SJHS’s Centre for Integrated Care has launched.
Attendees at the session included healthcare leaders, patient advisors and front-line staff from Kingston Health Sciences Centre, Peterborough Regional Health Centre, Peterborough County/City Paramedics, Peterborough Family Health Team, Mississauga Halton LHIN, and Guelph General Hospital.
Since 2012, St. Joseph’s Health System has pioneered Integrated Care in Ontario in partnership with patients, front line staff, health care delivery partners, as well as the Ministry of Health and local funding bodies. Integrated Comprehensive Care is an evidence-based model of Integrated Care that supports patients with One Team, One Record, One Number to Call, 24/7.
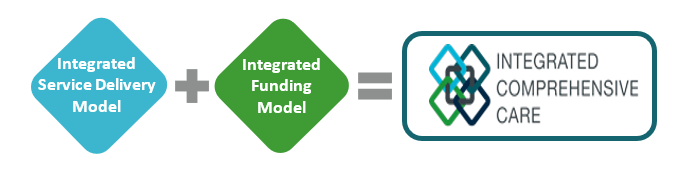
ICC is enabled by a co-designed integrated service delivery model and an integrated funding model, which we refer to as One Fund. Our focus is to make the patient experience as seamless as possible while utilizing existing resources across the healthcare continuum, to deliver an integrated and comprehensive care experience. ICC is sustainable, transformational system change enabled by evidence-based integrated service delivery and funding model.
“With over 17,000 patients served to date through the ICC program and savings of up to $4,000 per patient, it is essential to share practical advice on how to replicate this success. To date, we have coached over 30 organizations and continue to be the resource for our health system colleagues seeking advice and support on how to implement integrated care,” says Fraser Edward, Vice President, Partnerships and Business Development, St. Joseph’s Health System. “These Integrated Care Discovery Sessions are a great way for us to share key learnings with other healthcare leaders, patient advisors and frontline staff; and provide a platform for discussion and collaboration.”
The session took place at St. Joseph’s Healthcare Hamilton, in partnership with St. Joseph’s Home Care with speakers including ICC coordinators, clinical programs, finance, digital solutions and our front-line home care team. Our group shared the knowledge gained from their practical experience launching and working with this model.
Topics included how to establish a foundation of trust through co-designing care paths with patients, staff and physicians; the role digital health technology play in Integrate Care; and how to build and manage an Integrated Funding model. The session also included a virtual visit demonstration with ICC patient ‘Georgia’ and the opportunity to hear her perspective on the impact of the program.
Throughout 2020, monthly Integrated Care Discovery Sessions will be held at St Joseph’s Healthcare Hamilton, open to healthcare organizations interested in learning about evidence-based models of Integrated Care.
To secure your spot at the next ICC Discovery Session, please contact:
Fraser Edward
Vice President, Partnerships and Business Development,
St. Joseph’s Health System
Find out more about the ICC program and the Centre for Integrated Care.







