Representatives from healthcare organizations across the province gathered on January 23, 2020, to learn about St. Joseph’s Health System (SJHS)’s Integrated Comprehensive Care (ICC) program and how evidence-based models of Integrated Care could be applied in their organizations to support their Ontario Health Teams. The event is the first in a series of educational seminars, called Integrated Care Discovery Sessions, that SJHS’s Centre for Integrated Care has launched.
Attendees at the session included healthcare leaders, patient advisors and front-line staff from Kingston Health Sciences Centre, Peterborough Regional Health Centre, Peterborough County/City Paramedics, Peterborough Family Health Team, Mississauga Halton LHIN, and Guelph General Hospital.
Since 2012, St. Joseph’s Health System has pioneered Integrated Care in Ontario in partnership with patients, front line staff, health care delivery partners, as well as the Ministry of Health and local funding bodies. Integrated Comprehensive Care is an evidence-based model of Integrated Care that supports patients with One Team, One Record, One Number to Call, 24/7.
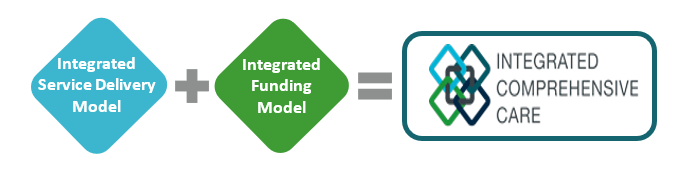
ICC is enabled by a co-designed integrated service delivery model and an integrated funding model, which we refer to as One Fund. Our focus is to make the patient experience as seamless as possible while utilizing existing resources across the healthcare continuum, to deliver an integrated and comprehensive care experience. ICC is sustainable, transformational system change enabled by evidence-based integrated service delivery and funding model.
“With over 17,000 patients served to date through the ICC program and savings of up to $4,000 per patient, it is essential to share practical advice on how to replicate this success. To date, we have coached over 30 organizations and continue to be the resource for our health system colleagues seeking advice and support on how to implement integrated care,” says Fraser Edward, Vice President, Partnerships and Business Development, St. Joseph’s Health System. “These Integrated Care Discovery Sessions are a great way for us to share key learnings with other healthcare leaders, patient advisors and frontline staff; and provide a platform for discussion and collaboration.”
The session took place at St. Joseph’s Healthcare Hamilton, in partnership with St. Joseph’s Home Care with speakers including ICC coordinators, clinical programs, finance, digital solutions and our front-line home care team. Our group shared the knowledge gained from their practical experience launching and working with this model.
Topics included how to establish a foundation of trust through co-designing care paths with patients, staff and physicians; the role digital health technology play in Integrate Care; and how to build and manage an Integrated Funding model. The session also included a virtual visit demonstration with ICC patient ‘Georgia’ and the opportunity to hear her perspective on the impact of the program.
Throughout 2020, monthly Integrated Care Discovery Sessions will be held at St Joseph’s Healthcare Hamilton, open to healthcare organizations interested in learning about evidence-based models of Integrated Care.
To secure your spot at the next ICC Discovery Session, please contact:
Fraser Edward
Vice President, Partnerships and Business Development,
St. Joseph’s Health System
Find out more about the ICC program and the Centre for Integrated Care.
The model of bundled care sees different groups of providers band together, share accountability and care for the patient throughout the entire journey.
July 24, 2019 By Joanna Frketich , Grant LaFleche
The Hamilton Spectator and St. Catharines Standard

HAMILTON, ON- JUNE 17- Susan Apro helps her mother Pat Coffer, 94, into bed in Apro’s livingroom where Coffer spends 18-20 hours a day sleeping. Coffer was relatively healthy – gardening and walking – until she started having heart issues in April . It’s hard to guess what the journey of patients like Pat Coffer will look like after the Progressive Conservative’s massive health-care restructuring, but the goal is for it to resemble bundled care. bundled care attempts to bridge the gaps that often leave patients lost by never handing the patient off from one service to another, making life for people like 94-year-old Pat Coffer, a little bit easier. June 17, 2019. John Rennison/The Spectator
Something as simple as a phone number has made it doable for Susan Apro to care for her 94-year-old mother at home.
Those 10 digits mean help from St. Joseph’s Healthcare is just a call away for the 70-year-old daughter who is taking on the daunting task of caregiver after her fiercely independent mom, Pat Coffer, developed untreatable heart issues and an aneurysm in April that has left her severely debilitated.
“It means the world to me,” said Apro. “For mom to come home, the burden has all fallen on me … I don’t know what the heck I’m doing.”
The trusted voice on the other end of the line can send a nurse or personal support worker to the East-Hamilton house outside of the usual home-care schedule. Another day, Apro could be asked to send a picture of an emerging bed sore to get instructions on what to do.
“I didn’t have to scramble to get anyone to come into the home,” said Apro. “We can call this number any time.”
Never having to navigate the health-care system alone is the foundation of the highly successful pilot program called bundled care or integrated comprehensive care, introduced by St. Joseph’s in 2012.
“My mom made me promise that she would never go in a nursing home, so as long as I’m able, I’ll keep my mom home, looking after her,” said Apro. “With this program, I have that support behind me.”
It’s hard to guess what a patient’s journey will look like after the Progressive Conservative’s massive health-care restructuring, but the goal is for it to resemble bundled care.
“It is a highly respected model that this plan mimics,” says Donna Skelly, Conservative MPP for Flamborough—Glanbrook. “It has been very successful in Hamilton. It’s a model that we are, in essence, replicating with this new approach to health-care delivery.”
The health-system revamp came into effect June 6 under the Connecting Care Act. An investigation by The St. Catharines Standard and The Hamilton Spectator provides the most comprehensive coverage to date of the overhaul, considered the biggest change since Medicare.
The plan, announced in February, puts a super agency named Ontario Health in charge of the entire health-care system — from hospitals to community care to organ donation to cancer care. It will oversee dozens of regional groups, called Ontario Health Teams, made up primarily of health and social service organizations working together to integrate services locally and help area residents navigate the system.
As the Conservatives undo many of the previous governments’ health-care reforms, primarily local health integration networks (LHINS), there is some irony that a program championed by the Liberals is the prototype for the latest round of health-care restructuring.
Similar to the planned Ontario Health Teams, the bundled care model sees different groups of providers band together, share accountability and care for the patient through the entire journey. There is one pot of money split between all the services, increased use of technology and a navigator to guide patients’ through the system.
“Even family docs have trouble navigating the system,” said Dr. Tom Stewart, CEO of St. Joseph’s and Niagara Health. “We need to make it easier.”
Stewart himself admits he was worried when his father’s lung cancer surgery was scheduled on a Friday at the Hamilton hospital he now leads.
“You’re always a little nervous sending people home on Friday because you’re not sure their home-care team is going to show,” he said. “There is not that point of accountability. It’s a fragmented system.”
Bundled care attempts to bridge the gaps that often leave patients lost by never handing the patient off from one service to another.
Planning starts at admission — or even before for scheduled procedures — so services needed, both in and out of hospital, are pre-arranged and ready to go when needed.
Discharge is not when the patient leaves the hospital but roughly 60 days after going home with one team of providers responsible for the patient’s care from start to finish. The team could include doctors, nurses, physiotherapists, occupational therapists, social workers, dietitians, respiratory therapists, speech and language pathologists and personal support workers. Ideally, the patient meets as much of the team as possible before leaving the hospital.
Most important, there is one point of contact called a care co-ordinator who arranges what’s needed, oversees the care and helps the patient navigate the system.
“We would refer and set up all their services at home,” said Heather Paterson, Niagara Health’s chief nursing officer and director of patient care. “Our care co-ordinator follows (the patient) from hospital to home.”
Patients get a number to call 24-7 where co-ordinators are on standby to stick handle any issues.
Members of the team, such as specialists, can be accessed through technology, which is the type of “virtual visit” recommended by the Premier’s Council on Improving Health Care and Ending Hallway Medicine in its June report as a way to cope with the increasing demands of an aging population.
Stewart’s dad was able to get immediate answers from his doctors without leaving home when there were potential issues with his surgical wound.
“I’m a doctor, and I would have quite honestly said, ‘Go back to emerg,'” said Stewart. “He ends up calling a number and sending a picture of the wound from home with technology, and the doctors say, ‘This is normal. Don’t worry about it.’ That prevents an emerg admission, so you can see how you can start to improve the system.”
Stewart says the program’s three major pillars are one multidisciplinary team, one medical record and one number for patients to call.
The program now stretches from Niagara to Kitchener and has expanded to include chronic lung disease, congestive heart failure, lung cancer surgery, hip and knee replacements, peritoneal dialysis and mental health and addictions. In the fiscal year that started April 1, it is expected to expand to all patients undergoing planned and scheduled surgeries at St. Joseph’s.
So far, 17,000 area patients have received bundled care. Its success was highlighted by the Premier’s Council. Its June report states the program reduced length of hospital stay by 1.26 days on average, reduced costs within 30 days by $2,110 and within 90 days by $3,035.
In addition, 87 per cent of surveyed patients said they felt they were involved and informed in their care.
“The vast majority are saying it’s way better,” said Stewart. “The health-care workers are happier and home-care workers are telling us they feel they can get a nurse or doctor at the hospital easier now, and they feel part of the same team. Caregivers, the patients and their families are a lot more happy.”
St. Joseph’s reports up to a 30-per-cent reduction in emergency visits and hospital readmission rates
At Niagara Health, the readmission rate has fallen to 15 per cent from 19 per cent three years ago, when the program started. The number of patients having to visit the emergency room after discharge also fell over the same period to 32 per cent from 38 per cent.
“By offering the support and building capacity in the community, we are able to manage patients and give them access to care they might not have had,” Paterson said.
It was a lifeline for Apro after her active mom went from gardening and walking to spending most of her time in bed.
She wouldn’t have known where to turn if the program hadn’t arranged for a hospital bed, walker and commode chair to be sent to her house so her mom could live on the main floor. Making it more difficult is that Coffer hasn’t had a family doctor since hers retired.
“My mom has never been sick, and all of a sudden, she’s got these heart issues and she can’t even wash herself,” said Apro. “It’s very upsetting, and it’s a lot of work to take on, but I wouldn’t let anyone else do it.”
The program isn’t perfect. Its major weakness is primary care isn’t involved at all, leaving patients vulnerable after discharge from bundled care.
“There’s got to be that hand off,” said Dr. David Price, head of family medicine at McMaster University. “If you don’t integrate that then they fall through the cracks.”
Bundled care is also too narrow in scope, says Rob MacIsaac president and CEO of Hamilton Health Sciences.
“From my perspective, it doesn’t make a lot of sense to limit it to certain patient populations that are defined by their illnesses,” he said. “I think it would be much better if we could open it up.”
Under Ontario Health Teams, this model would significantly expand to eventually cover all patients and not just those transitioning from hospital to home.
“It will improve patient care by connecting care,” Health Minister Christine Elliott said on a July 18 conference call with health care workers. “People are discharged from hospital, and those people feel like they are shut out of their own health care system and have to fight their way back in.”
She said patients need to know their after-hospital care will continue at home, know how that care works and when and how they can access it.
Even the CEO of the regional network being dismantled by the restructuring thinks patients will be better off in the end.
“While we know these proposed changes will take time, when fully realized, patients, families and caregivers will have access to faster, better and more co-ordinated services,” said Donna Cripps, CEO of the Hamilton Niagara Haldimand Brant LHIN, which includes Burlington.

HAMILTON, ON- JUNE 17- Susan Apro has her mother Pat Coffer, 94, living in her livingroom where Coffer spends 18-20 hours a day sleeping. Coffer was relatively healthy – gardening and walking – until she started having heart issues in April . June 17, 2019. John Rennison/The Spectator
It is expected to take years before the monumental changes envisioned by the Conservatives are in place.
“You just can’t change a system as big as health care on a dime,” said Paul Johnson, who is representing the city in the Hamilton Ontario Health Team application.
The government also has to be careful not to disrupt care during the changes.
“It has a lot of promise but, in the meantime, there are going to be things that have to be done to keep the health system functioning while facing some very serious challenges,” said Anthony Dale, president and CEO of the Ontario Hospital Association.
The Ontario Health Coalition worries those pressing issues, like overcrowded hospitals, inadequate home care and shortages of long-term care, will fall by the wayside during the overhaul.
“The whole attention of the health-care system now has turned to restructuring and will be for years,” said executive director Natalie Mehra. “I fear for how long it is going to take to go through all of this.”
It’s expected the health-care changes will happen so gradually that patients won’t ever see a big bang where suddenly the health-care system is turned on its head.
“You won’t notice much of a difference in the first week or month or even the first six months,” said Price. “I hope when we look back in three to five years, we will see difference.”
For the most part, patients will continue to interact with the health-system as normal.
“The message we’re communicating … is business as usual,” said Dr. Ralph Meyer, vice-president of oncology and palliative care at HHS and regional vice-president of Cancer Care Ontario. “We’ll evolve as the system evolves.”
The LHIN says its continuing to do the same work it has always done, even as its board has been dismantled and back-office jobs eliminated.
“Home and community care continues as before, and there are no changes to the long-term care home placement,” said Cripps. “People can continue to contact their home- and community-care providers as normal to access the care they need.”
The Canadian Union of Public Employees (CUPE) says the slow change will be hard for health-care workers, particularly in sectors where their roles are expected to dramatically shift.
“For the people who work for the LHINs, nobody knows really what will happen to them,” said Michael Hurley, president of the Ontario Council of Hospital Unions, which is part of CUPE. “They are expected to soldier on; they are not asked for their input, and they are not valued.”

Never having to navigate the health-care system alone is the foundation of the highly successful pilot program called bundled care or integrated comprehensive care, introduced by St. Joseph’s in 2012, which makes it much easier for Susan Apro to care for her mother Pat Coffer. | John Rennison, The Hamilton Spectator
The health-care system is split on how to respond to the changes, with lines drawn between those planning to protest and those hoping to be among the first to adopt the new system.
“We will fight the legislation,” said Mehra. “It’s undemocratic and it’s dangerous.”
The Ontario Health Coalition wants public hearings across the province so Ontarians can have their say.
“The government needs to hear from Ontarians about the real, on-the-ground impacts of what they have created,” said Mehra. “Slow down and listen to people.”
CUPE agrees that the lack of consultation with the public and health-care workers is a top concern.
“I would really appreciate it if this government would stop this process and have a genuine dialogue with people,” said Hurley.
The Ontario Nurses’ Association has started a campaign with the slogan, “Don’t let Doug Ford wreck health care” that urges people to email the premier, the health minister and their MPP.
“This chaotic overhaul of health care is going to take years and cost millions, and there’s no guarantee it will add one single hour of direct care, and it won’t add any of the skilled caregivers who are needed so urgently,” states the campaign.
“The whole attention of the health care system now has turned to restructuring and will be for years. I fear for how long it is going to take to go through all of this,” says Natalie Mehra, the Executive director of Ontario Health Coalition. | Chris Young, The Canadian Press
Unifor had a phone-in town hall for its members about the restructuring and has started a leaflet campaign.
“Wherever we can, we’re going to join in the fight,” said regional director Naureen Rizvi. “People are very angry.
A rally at Queen’s Park April 30 led by the Ontario Health Coalition drew thousands of protesters.
“They’re saying it’s going to be a streamlined system, but I don’t see how they’ve put a model together that actually achieves that,” said Andrea Horwath, Hamilton Centre MPP and leader of the NDP.
On the flip side, Niagara, Hamilton and Burlington health and social service organizations have applied to be early adoptors of the changes by proposing Ontario Health Teams, which are expected to transform the local system. All three groups were informed July 18 that their proposals are moving to the next stage of application.
“In Hamilton, we are in a really good spot to respond to this call,” said family physician leader Price.
Health leaders see it as a logical extension of work that has been going on for years in this area.
“We think we’re ready in Burlington and that we could move forward quite quickly,” said Eric Vandewall, CEO of Joseph Brant Hospital. “We’ve got a lot of enthusiasm around the table and a lot of support for moving forward.”
The province plans to learn from the first Ontario Health Teams to tweak the restructuring as problems are found.
“We have to be looking at these early adopters” said Sue VanderBent, CEO of Hamilton-based Home Care Ontario. “They’re our little petri dish where we try some things and we watch what happens and we learn from that.”
But the experiment really started in Hamilton, with bundled care spreading out over the years to Niagara, Burlington and all of the acute care hospitals in the LHIN and beyond.
“It made a huge difference for me,” said 93-year-old Helen Greves, who got bundled care in February after being released from the Niagara Health cardiac unit in St. Catharines.
While she was part of the program because of her heart condition, bundled care was able to have the flexibility to also look after an unrelated ankle injury from a fall at her Niagara-on-the-Lake home shortly before she went into hospital that has made going out for medical treatment even more difficult.
“Well, at 93 I qualify as elderly, I think,” said Greves. “So I really needed the help.”

Eric Vandewall, CEO of Joseph Brant, says a Burlington mental health partnership has increased access to a wide variety of providers. “We’ve eliminated the feeling patients have about not knowing where to go and being bounced around.” | John Rennison, The Hamilton Spectator
What will your care look like?
No one knows yet exactly what care will look like after the health-care overhaul, but a number of area programs give a potential glimpse of the future.
Joseph Brant Hospital
A Burlington mental health partnership gives patients one point of access to a wide variety of providers so they don’t have to navigate the services on their own. Instead, they are directed to the agency best able to meet their needs.
“Historically we did not operate together,” said Eric Vandewall, CEO of Joseph Brant. “Patients would not know how to access service, which is the right provider, and things were not always timely.”
A second program for chronic obstructive pulmonary disease provides patients with a phone number to call when they need guidance and help navigating the system.
A group for those recovering from hip- and knee-replacement surgery allows patients to do rehab, which would normally be provided at home alone, in a clinic with other patients instead. It’s cheaper, has better outcomes and higher patient satisfaction because it provides peer support and motivation.
“All of this is really about working differently with our community-care providers,” said Vandewall about the various programs. “We’ve increased access, we’ve eliminated the feeling patients have about not knowing where to go and being bounced around, they have timely support, and we’ve been able to reduce wait times significantly.”
Niagara Emergency Medical Services
Non-urgent ambulance calls are visited by Mobile Integrated Health Response Teams in Niagara to connect them with the care they need in the community without going to the hospital.
The teams, made up of EMS and providers in the community, were highlighted in June by the Premier’s Council on Improving Health Care and Ending Hallway Medicine for reducing transports to the emergency department by six per cent for those feeling generally unwell, five per cent for mental health issues and two per cent for falls.
• • •
Operation health care reform: Your guide to the series
The provincial government is undertaking a sweeping overhaul of the health-care system. The changes came into effect June 6 under the Connecting Care Act.
An investigation by The St. Catharines Standard and The Hamilton Spectator provides comprehensive coverage of the health reforms considered the biggest change since Medicare. A four-day, nine-story series looks into all aspects of the plan.
Under the plan, a super agency called Ontario Health will be in charge of the entire system from hospitals to community care to organ transplants to cancer care. It will also oversee dozens of regional groups named Ontario Health Teams that will align health and social service organizations to work together to integrate services and help patients navigate the system.
July 2, 2019 – Canadian Healthcare Technology
HAMILTON, ONT. – St. Joseph’s Health System (SJHS) is using video visits to connect clinicians with discharged surgical patients at home.
The video-based care builds on St. Joseph’s use of one phone-number access to an integrated care team, around the clock, for discharged patients and provides another dimension of support in their homes.
The video service was launched in January of this year, in conjunction with the Ontario Telemedicine Network (OTN), St. Joseph’s Healthcare Hamilton (Hospital) and St. Joseph’s Home Care, and started with patients discharged from thoracic, hip and knee surgeries.
Once at home, the patients can use computers, tablets or smartphones to interact visually and by voice with a coordinator who is able to answer their questions and can connect them with other members of the care team. Virtual “face-to-face” visits can be scheduled with clinicians, home care nurses, and the patients access these visits through a digital patient portal called MyDovetale.
Since 2012, St. Joseph’s has pioneered a new model of care called Integrated Comprehensive Care (ICC), which gives patients and their families access to One Health Team, One Digital Record, and One Number to Call, 24/7.
Patients first meet their ICC coordinator while in hospital, to receive discharge information, learn about the ICC program and support they will receive at home. Once the patient is in the community, the ICC team uses ‘virtual rounds’ to discuss patients and their care plan together.
Everyone is in the loop and patients don’t repeat their information every time.
“We’re the first Hospital in Ontario to use integrated virtual care software, outside of the Ontario Telemedicine Network OTNhub, to support our patients,” said Andriana Lukich, program manager.
The video service is integrated with the hospital’s new Epic information system (branded as Dovetale), so that clinical records, including diagnostic images and lab test results, can be pulled up and shared while the meeting is going on.
Clinicians can write notes and update the records while they’re conducting the video encounters. The proof of concept is now being expanded to new patient populations at St Joseph’s and has paved the way for OTN’s new Partner Video Project initiative, Lukich said.
The pilot project discovered that virtual visits are not for everyone. Some patients struggled with the technology, and small factors like lighting and avoiding the mute key on a phone could hinder interactions with clinicians.
For that reason, the standard telephone is available for all patients – it’s still the easiest way to reach the ICC team, any time night or day.
Secure Messaging through the MyDovetale patient portal is also offered.
Lukich and hospital Chief Information Officer Tara Coxon discussed St. Joseph’s virtual care solution at the Technology & the Future of Healthcare conference, held in Hamilton in May.
The ICC program has been further enabled by St. Joseph’s Healthcare Hamilton’s implementation of Epic (Dovetale), which went live at St. Joseph’s in December 2017. At that time, said Coxon, St. Joe’s became a digital hospital and jumped to HIMSS EMRAM Stage 6. “Previous to that, we were at EMRAM 1.2,” she said. “It was an over-night transformation.”
The Epic implementation at St. Joseph’s Healthcare Hamilton was named Dovetale to signify the joining of technology with compassion. The system is helping to smooth out some of the pain points in Ontario’s healthcare system, specifically the hand-offs that occur when patients move from one level of care to another.
In one recent instance, a lung cancer patient who underwent surgery at St. Joseph’s was discharged home to Beamsville, only to discover that his wound seemed abnormal. He was worried it might have become infected.
He contacted his ICC coordinator at St. Joseph’s using the one-number service, and she instigated an ad hoc video visit to view the wound in real-time and determined that the patient should receive care right way.
This was arranged through St. Joseph’s Home Care, and on the same day, a visiting nurse travelled to the patient’s home and changed his wound dressings. She also updated his chart, right on the spot.
St. Joseph’s is making medical records available to the patients themselves through the use of a portal – called MyDovetale. “We were hearing that patients wanted better access to their records and that they wanted their records to be accurate and accessible throughout the system,” said Lukich.
In the summer of 2018, St. Joseph’s went live with the MyDovetale portal, extending it to patients in the mood disorder and kidney transplant clinics.
Patients can access their records on any platform, but it’s been found that smartphones are now the most popular device. Access can be given to family members, loved ones and members of care teams. Lukich said that 88 percent of patients report that MyDovetale has allowed them to take better care of themselves. Meanwhile, the video visit service has saved some patients two to three hours of travel time.
Patients have been asking for enhancements to the MyDovetale solution – in particular, they’d like to see prescription renewals and diagnostic imaging reports made available on the system.
MyDovetale will soon be rolled out to 80,000 more patients – an organization-wide rollout.
According to St. Joseph’s, the ICC program has resulted in a savings of up to $4,000 per patient, a 30 percent reduction in emergency department visits and 30 percent reduction in hospital readmissions with a 98 percent patient satisfaction approval rating. It’s doing this by enabling patients to stay comfortably in their homes, getting the reassurance or care they need without visiting the hospital.
The program has been so successful that Ontario’s health ministry would like to expand it to other healthcare providers.
“Already, St. Joseph’s has coached over 30 other organizations on how they might implement an ICC model of their own,” commented Fraser Edward, VP partnerships at SJHS.
“We have established the Centre for Integrated Care to help support Ontario Health Teams and other healthcare providers wrap physical and virtual care around the needs of patients and their families.” For more information, see: www.sjhs.ca/integratedcare/cic/
By: Melissa Farrell, President, St. Joseph’s Healthcare Hamilton
We are delighted to announce that St. Joseph’s Healthcare Hamilton has received our final decision from the Accreditation on-site survey in May and have been granted a decision of: Accredited with Exemplary Standing – the highest rating for a Canadian hospital.
Given the multiple challenges in health care today it is truly an honour to receive the highest level of Accreditation, a testament to the dedication and determination of everyone at St. Joe’s to continuously enhance the quality of care we provide to our patients and our community. We would like to congratulate each and every one of you on this wonderful achievement. I also want to point out St. Joe’s received “Exemplary Standing” in the previous accreditation – achieving this again is a sign of the outstanding commitment to the highest standard of care.
Accreditation is a genuine opportunity to evaluate our care, identify areas for improvement and celebrate our achievements. The final decision indicates we have met and often exceeded almost all national standards of care. Where opportunities for improvement were identified, we have already started to work on these areas. The final report will be available online on our here as it becomes available.
The survey team particularly complimented St. Joe’s on:
- The commitment and passion of our staff, leadership, physician team, volunteers and Board of Governors
- Our commitment to quality and safety
- Our community focus
- Our work on partnering with patients and families
- The many program-specific accomplishments
As you are aware, the Accreditation process requires our continued vigilance and continuous quality improvement to ensure that we are sustaining our progress in providing excellent care to our patients. Take pride in this accomplishment and be assured that all of the hard work and challenges we undertake over the next few years will continue to demonstrate our commitment to providing high quality, safe and compassionate care.
We would also like to extend a special thank you to the Accreditation steering committee leaders and Patient and Family Advisors whose counsel was instrumental in guiding us through processes to achieve a successful outcome.
Sincerely,
Melissa Farrell, President, St. Joseph’s Healthcare Hamilton
May 29, 2019
HAMILTON ON – Hamilton philanthropists Charles and Margaret Juravinski will create an endowment of more than $100 million to support researchers across Hamilton Health Sciences, McMaster University and St. Joseph’s Healthcare Hamilton.
Their estate gift is one of Canada’s largest ever legacy gifts and will provide up to $5 million a year to the institutions, in perpetuity.
“It brings us great pleasure to think that when we are gone, our legacy to this community may be measured in the good health of those who come after us,” the Juravinskis said in a letter to the community released today. “As a couple, our most important lesson has been this: the greatest pleasure in life and the most powerful force for good in the world is sharing.”
The endowment will create the Juravinski Research Centre, which will equally support Hamilton Health Sciences, McMaster University and St. Joseph’s Healthcare Hamilton by funding health research in a variety of areas including cancer, mental health, lung and respiratory care, and diseases of aging.
The Juravinskis, who have called Hamilton home for decades, are generous benefactors to health care, education and research in the city. They have given more than $50 million to Hamilton organizations, which includes support for the Juravinski Hospital and Cancer Centre at Hamilton Health Sciences, the Margaret & Charles Juravinski Education, Research & Development Centre at McMaster University and the Margaret & Charles Juravinski Centre for Integrated Healthcare and the Juravinski Innovation Tower at St. Joseph’s Healthcare Hamilton.
A Historic Hamilton Gift
“The health of generations of Canadians will be positively impacted by this wonderful legacy gift from Charles and Margaret Juravinski. In making this gift, they also helped inspire and enable our three organizations to collaboratively address some of the most important health issues of our time.” – Rob MacIsaac, President & CEO, Hamilton Health Sciences
“McMaster had already started talks with Hamilton Health Sciences and St. Joseph’s about how we could create new dimensions to our research partnerships to deliver even more to our community, when I received a call from Charlie Juravinski. He was very excited to explore how he and Margaret could leave a legacy that would improve the health
of people in Hamilton and around the world by supporting research. We will be eternally grateful for Charlie and Margaret’s vision and their confidence in our world class researchers’ ability to have deep and long-lasting impact in many critically important areas of health research.” – Dr. Paul O’Byrne, Dean and Vice-President, Faculty of Health Sciences, McMaster University
“Charles and Margaret Juravinski’s visionary gifts have forever changed health care in Hamilton and their legacy of giving will continue thanks to their investment in world-class research. By enabling collaborative research into mental health care, lung and respiratory health, oncology, and diseases of aging, the Juravinskis’ gift will impact not only patients and families in Hamilton, but countless others around the world for generations to come.” – Dr. Thomas Stewart, President & CEO, St. Joseph’s Health System
About the Juravinski Research Centre
- A research collaboration between Hamilton Health Sciences, McMaster University, St. Joseph’s Healthcare Hamilton, St. Joseph’s Healthcare Foundation, Hamilton and Hamilton Health Sciences Foundation
- The Centre will support areas of research including cancer, mental health, lung health/respirology and diseases of aging (e.g. Alzheimer’s disease and macular degeneration)
- Together, the partners will engage in collaborative, strategic projects that are focused on health-related research enhancing the health and prosperity of all of our citizens
- An eight-member Steering Committee will be responsible for setting all priorities and programs to be undertaken by the Juravinski Research Centr
Charles and Margaret Juravinski – A Legacy of Leadership
- Charles, 89, and Margaret, 87
- Charles (born in Blaine Lake, SASK) and Margaret Juravinski (born in Hamilton, ON) grew up knowing true poverty and hardship.
- Charles, born within days of the 1929 stock market crash, knew what it was like to live without work, money, heat and running water. His family moved to Hamilton when he was a child. His professional career evolved after he first worked at a construction company and then went on to own a series of businesses, which included a gas station and a development company.
- Charles and Margaret built and managed Flamboro Downs race track for 27 years, selling it in 2002 to Magna Entertainment.
Links to video
A video message from the Juravinkskis
A video message from Dr. Thomas Stewart, President & CEO of St. Joseph’s Health System
The Institutions
Hamilton Health Sciences
Hamilton Health Sciences (HHS) is the only hospital system in Ontario providing specialty care to people throughout the entire life cycle, from pre-birth to old age. HHS serves the densely populated south central region of Ontario and is also a referral centre for patients from elsewhere in the province.
With five hospitals (Hamilton General Hospital, Juravinski Hospital and Cancer Centre, McMaster Children’s Hospital, St. Peter’s Hospital and West Lincoln Memorial Hospital) and six specialized healthcare facilities, HHS has the largest hospital-based workforce in Ontario: 15,000 staff, physicians and volunteers.
In addition to providing excellent patient care, Hamilton Health Sciences’ mission includes advancing health care through education and research. In affiliation with McMaster University and other educational institutions, HHS is helping to train the next generation of caregivers. It has also become an international leader in hospital-based research and is recognized as one of the top four healthcare research institutions in Canada. More than 2,000 investigators and research staff at HHS work together to attract $170 million in research funding annually.
Hamilton Health Sciences Foundation
Hamilton Health Sciences Foundation provides vital funding to enable the best possible patient care. We inspire and motivate gifts that fund medical equipment and patient amenities, innovative research initiatives, essential redevelopment of clinical care spaces, and the education and training of health care providers. As a registered charitable organization, we proudly support patients and families across south-central Ontario, and from outside the region, who receive specialized care at Hamilton Health Sciences including Hamilton General Hospital, Juravinski Hospital and Cancer Centre, McMaster Children’s Hospital, and St. Peter’s Hospital. The associated programs at the Regional Rehabilitation Centre, McMaster University Medical Centre and Ron Joyce Children’s Health Centre are also included.
McMaster University
McMaster University is Canada’s most research-intensive university and is consistently ranked as one of the world’s Top 100 universities. Together, our researchers, students and staff advance human and societal health and well being, creating a Brighter World.
St. Joseph’s Healthcare Hamilton
St. Joseph’s Healthcare Hamilton (SJHH) is a leading research and academic health science centre located in the heart of Hamilton, Ontario. It is a pioneer of the Integrated Comprehensive Care model, a leader in patient-centred care, and a major provider of mental health and addiction services, respiratory care and kidney care, in addition to other acute care, surgical and outpatient services at its three distinct sites. SJHH is a member of the St. Joseph’s Health System, working in close partnership with St. Joseph’s Villa Dundas for long-term care, and St. Joseph’s Home Care.
St. Joseph’s Healthcare Foundation
Since 1970, St. Joseph’s Healthcare Foundation has been proud to partner with the community to raise funds in support of the exceptional patient care, innovative research and education, and vital facility and equipment needs at St. Joseph’s Healthcare Hamilton.
In 2012, St. Joseph’s Healthcare Foundation became one of a selected group of charities across Canada to be accredited by Imagine Canada’s Standards Program. The program recognizes excellence in Canadian charities in five areas, including: board governance, financial accountability & transparency, fundraising practices, staff management, and volunteer involvement.
Publication: Council of Academic Hospitals of Ontario | May 9, 2019
Rheumatoid arthritis (RA) is an auto-immune disease that affects approximately 1 in 100 Canadians. RA is caused by a malfunction of the body’s own immune system. The disease is characterized by joint inflammation that causes pain, stiffness, and swelling. Joint degradation occurs as a result of the immune system’s attack on the lining of the joints.
Early signs of RA can be vague, such as feeling tired and unwell, accompanied by sore joints. As the disease progresses, more joints may become affected. Detecting RA in its early stages is a major factor in the successful treatment of the disease. The window to achieve remission, thereby preventing permanent damage to the joints, is an estimated 6-12 months, and this narrow timeframe presents a challenge.
Dr. Maggie Larché is a clinician-researcher at St. Joseph’s Healthcare Hamilton. For years, Dr. Larché has been at the forefront of advancing the use of ultrasound in the diagnosis and treatment of RA. Dr. Larché also teaches musculoskeletal ultrasonography to medical trainees and clinicians in an effort to expand use of this diagnostic technique.
Research on the feasibility of ultrasound for RA diagnosis conducted by Dr. Larché and her colleagues is transforming the field of rheumatology in Canada. Though the technique may require longer clinical visits for patients at the point of care, its ability to enhance early detection and monitoring will help more Canadians start treatment sooner and avoid permanent damage to their joints. Not only does this reduce the health care resources needed to treat chronic RA, it assists in improving patient quality of life.
“We know that ultrasound can detect RA sooner than clinical methods, and an earlier diagnosis can have a significant impact on a patient’s recovery and overall quality of life,” explains Dr. Larché. “My colleagues and I have promoted the use of ultrasound in diagnosing and monitoring patients with RA, as well as increased the use to ultrasound training for health care providers in Canada.”
Overall, there are many advantages of using ultrasound over other imaging methods. Ultrasound is a non-invasive, radiation-free, portable, and inexpensive tool for diagnosing RA. In addition, diagnosis occurs in real-time with the patient, unlike an MRI or CT scan.
“I was diagnosed with RA in my hands. The treatment for RA involves injections to reduce the inflammation that causes pain. Her use of ultrasound to pinpoint the problematic spots of my hands allows her to find the best place for each injection, improving the effectiveness of the treatment. Dr. Larché has given me the use of my hands, which has greatly improved my quality of life,” said Margaret Clark, patient and research participant.
St. Joseph’s Healthcare Hamilton is one of Ontario’s 23 research hospitals that contribute to a healthier, wealthier, smarter province. Look for other RESEARCH SPOTLIGHT posts on our Healthier, Wealthier, Smarter blog or join the conversation about why health research matters for Ontario on Twitter, using the hashtag #onHWS.

