
(HAMILTON, NIAGARA) – NOVEMBER 12, 2020 – COVID Care @ Home is a new model of care delivered by St. Joseph’s Home Care (SJHC), in partnership with St. Joseph’s Health System (SJHS), Niagara Health and community partners that connects patients to care wherever they are, whenever they need it.
Starting at St. Joseph’s Healthcare Hamilton and Niagara Health, with rapid expansion to Kitchener, this new model of care for COVID patients will provide 24/7 access to high-quality care from one integrated team in the home and in community settings like retirement homes, shelters and hospices.
COVID Care @ Home is a uniquely designed program intended for those with a confirmed COVID diagnosis who do not require hospitalization. Complimenting existing local COVID initiatives, the program will support integrated care at home, early discharge from hospitals with supports and help to prevent hospitalization. It will also help to prevent outbreaks by providing Infection Prevention and Control (IPAC) and coaching support for community congregate settings.
Patients will be assessed to determine what level of service will be provided. Vulnerable patients who are at risk of hospitalization and who require additional supports and services will have access to an integrated clinical care team, remote monitoring and at-home and virtual visits to support a safe recovery at home. This same model of care will be available to patients discharged from hospital so they can safely return home sooner.
This innovative, flexible model would provide COVID patients access to services that may not typically be within the scope of traditional home and community care supports. Patients will be cared for by one integrated team representing a variety of providers whose clinical decisions are empowered through the use of a single electronic patient record to support patients in the following ways:
- Virtual Care (phone, video and remote patient monitoring)
- One number to call 24/7
- One clinical team
- One electronic record
- System navigation / connection to social supports
- Access to specialists
- IPAC Support
St. Joseph’s Home Care will lead this innovative transformation to connect home care to a broad range of services for COVID patients and work in collaboration with other service provider organizations and primary care.
SJHS is one of the largest healthcare organizations in Canada, and the only system in Ontario delivering a full continuum of integrated health care services.
“We’ve learned a tremendous amount about COVID-19 over the last several months,” said Tom Stewart, St. Joseph’s Health System President and CEO and CEO of Niagara Health. “This new program builds on partnerships and learnings by increasing our focus on virtual care and specialized COVID care teams that crosses normal silos of care. This will help us through the second and future waves of the pandemic as well as prepare us for system transformation needed in healthcare.”
The program is designed to support older adults who are at greater risk of physical and mental health decline. Patients will be enrolled by the clinical teams at the time of their COVID 19 diagnosis.
The new model will also help to protect capacity in hospitals by expanding supports and services in the community through a dedicated team that will facilitate care at home, support safe discharges from hospital and limit unnecessary Emergency Department visits. This will help hospitals to maintain capacity and services during a second wave as well as continuing scheduled surgeries to reduce wait lists and backlogs.
About St. Joseph’s Home Care
Since 1921, St. Joseph’s Home Care has provided high quality, values-based home and community services in a spirit of compassion and dedication. We have evolved from a nursing agency to offering a much broader range of services, and our steadfast commitment to delivering exemplary client-focused care to the Hamilton community continues.
About St. Joseph’s Health System
St. Joseph’s Health System (SJHS) is one of the largest healthcare organizations in Canada, and is the only system in Ontario delivering a full continuum of health care services. SJHS is a globally recognized leader for innovation in models of patient-centred integrated care. SJHS has a unique partnership with Niagara Health to leverage each organization’s strengths to bring better care to the people in the communities we serve.
About Niagara Health:
Niagara Health is a regional healthcare provider with multiple sites and a growing network of virtual and community-based services. We provide a wide range of inpatient and outpatient services to more than 450,000 residents across Niagara, including Acute Care, Cancer Care, Cardiac Care, Complex Care, Emergency and Urgent Care, Kidney Care, Long-Term Care, Mental Health and Addictions, Stroke Care and Surgical Care.
About St. Joseph’s Healthcare Hamilton
As a premier academic and research healthcare organization, St. Joseph’s Healthcare Hamilton is committed to making a difference in people’s lives and creating a lasting future for our community through integrated health services and internationally recognized programs. Our threefold mission is to provide dynamic research, revolutionary methods in health sciences education and the highest standard of clinical care in a spirit of compassion, innovation and commitment.
For More Information:
Patrick Moore
Senior Public Affairs Specialist, St. Joseph’s Health System
M: 905.870.1293 | E: pmoore@stjoes.ca
Steven Gallagher
Communications Specialist, Niagara Health
P: 289-696-6767 | E: Steven.Gallagher@niagarahealth.on.ca
Representatives from healthcare organizations across the province gathered on January 23, 2020, to learn about St. Joseph’s Health System (SJHS)’s Integrated Comprehensive Care (ICC) program and how evidence-based models of Integrated Care could be applied in their organizations to support their Ontario Health Teams. The event is the first in a series of educational seminars, called Integrated Care Discovery Sessions, that SJHS’s Centre for Integrated Care has launched.
Attendees at the session included healthcare leaders, patient advisors and front-line staff from Kingston Health Sciences Centre, Peterborough Regional Health Centre, Peterborough County/City Paramedics, Peterborough Family Health Team, Mississauga Halton LHIN, and Guelph General Hospital.
Since 2012, St. Joseph’s Health System has pioneered Integrated Care in Ontario in partnership with patients, front line staff, health care delivery partners, as well as the Ministry of Health and local funding bodies. Integrated Comprehensive Care is an evidence-based model of Integrated Care that supports patients with One Team, One Record, One Number to Call, 24/7.
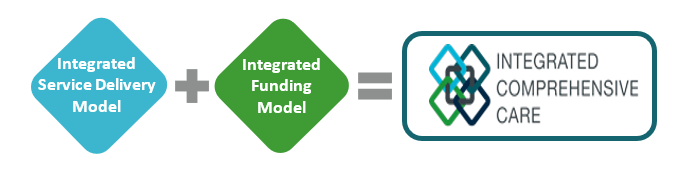
ICC is enabled by a co-designed integrated service delivery model and an integrated funding model, which we refer to as One Fund. Our focus is to make the patient experience as seamless as possible while utilizing existing resources across the healthcare continuum, to deliver an integrated and comprehensive care experience. ICC is sustainable, transformational system change enabled by evidence-based integrated service delivery and funding model.
“With over 17,000 patients served to date through the ICC program and savings of up to $4,000 per patient, it is essential to share practical advice on how to replicate this success. To date, we have coached over 30 organizations and continue to be the resource for our health system colleagues seeking advice and support on how to implement integrated care,” says Fraser Edward, Vice President, Partnerships and Business Development, St. Joseph’s Health System. “These Integrated Care Discovery Sessions are a great way for us to share key learnings with other healthcare leaders, patient advisors and frontline staff; and provide a platform for discussion and collaboration.”
The session took place at St. Joseph’s Healthcare Hamilton, in partnership with St. Joseph’s Home Care with speakers including ICC coordinators, clinical programs, finance, digital solutions and our front-line home care team. Our group shared the knowledge gained from their practical experience launching and working with this model.
Topics included how to establish a foundation of trust through co-designing care paths with patients, staff and physicians; the role digital health technology play in Integrate Care; and how to build and manage an Integrated Funding model. The session also included a virtual visit demonstration with ICC patient ‘Georgia’ and the opportunity to hear her perspective on the impact of the program.
Throughout 2020, monthly Integrated Care Discovery Sessions will be held at St Joseph’s Healthcare Hamilton, open to healthcare organizations interested in learning about evidence-based models of Integrated Care.
To secure your spot at the next ICC Discovery Session, please contact:
Fraser Edward
Vice President, Partnerships and Business Development,
St. Joseph’s Health System
Find out more about the ICC program and the Centre for Integrated Care.
As a result of our increasing focus on Ontario Health Teams and expansion of the Integrated Comprehensive Care initiatives, we are pleased to share the following leadership changes at St. Joseph’s Healthcare Hamilton and St. Joseph’s Villa Dundas.

Carolyn Gosse will be leaving her role as President of St. Joseph’s Villa Dundas, effective February 10th, 2020. She will continue her roles as President of St. Joseph’s Home Care as well as Vice President Integrated Care at St. Joseph’s Health System. In addition, she will continue as Lead of the Centre for Integrated Care.
Through our talent management process, John Woods has been identified as Carolyn’s replacement and will start as President of St. Joseph’s Villa Dundas on February 10th, 2020.

John joined St. Joseph’s Healthcare Hamilton in 1998 as Director of Strategic Planning and has held several leadership roles of increasing responsibility including; Director of Research Services, Director of Quality Planning & Performance, Director of Medical Affairs, Risk & Legal, Vice President of Strategic Initiatives for the St. Joseph’s Health System, and most recently, Interim President for St. Mary’s General Hospital in Kitchener.
John holds a Bachelor of Science in Physics from the University of London, a Master of Arts in Management Studies from Canterbury Christ Church University, and has completed the Advanced Health Leadership Program at the University of Toronto, Rotman School of Management.
John’s empathetic and relationship-based leadership style, with a focus on results, mission and strategy is highly valued and will be a great asset to the Villa.
July 2, 2019 – Canadian Healthcare Technology
HAMILTON, ONT. – St. Joseph’s Health System (SJHS) is using video visits to connect clinicians with discharged surgical patients at home.
The video-based care builds on St. Joseph’s use of one phone-number access to an integrated care team, around the clock, for discharged patients and provides another dimension of support in their homes.
The video service was launched in January of this year, in conjunction with the Ontario Telemedicine Network (OTN), St. Joseph’s Healthcare Hamilton (Hospital) and St. Joseph’s Home Care, and started with patients discharged from thoracic, hip and knee surgeries.
Once at home, the patients can use computers, tablets or smartphones to interact visually and by voice with a coordinator who is able to answer their questions and can connect them with other members of the care team. Virtual “face-to-face” visits can be scheduled with clinicians, home care nurses, and the patients access these visits through a digital patient portal called MyDovetale.
Since 2012, St. Joseph’s has pioneered a new model of care called Integrated Comprehensive Care (ICC), which gives patients and their families access to One Health Team, One Digital Record, and One Number to Call, 24/7.
Patients first meet their ICC coordinator while in hospital, to receive discharge information, learn about the ICC program and support they will receive at home. Once the patient is in the community, the ICC team uses ‘virtual rounds’ to discuss patients and their care plan together.
Everyone is in the loop and patients don’t repeat their information every time.
“We’re the first Hospital in Ontario to use integrated virtual care software, outside of the Ontario Telemedicine Network OTNhub, to support our patients,” said Andriana Lukich, program manager.
The video service is integrated with the hospital’s new Epic information system (branded as Dovetale), so that clinical records, including diagnostic images and lab test results, can be pulled up and shared while the meeting is going on.
Clinicians can write notes and update the records while they’re conducting the video encounters. The proof of concept is now being expanded to new patient populations at St Joseph’s and has paved the way for OTN’s new Partner Video Project initiative, Lukich said.
The pilot project discovered that virtual visits are not for everyone. Some patients struggled with the technology, and small factors like lighting and avoiding the mute key on a phone could hinder interactions with clinicians.
For that reason, the standard telephone is available for all patients – it’s still the easiest way to reach the ICC team, any time night or day.
Secure Messaging through the MyDovetale patient portal is also offered.
Lukich and hospital Chief Information Officer Tara Coxon discussed St. Joseph’s virtual care solution at the Technology & the Future of Healthcare conference, held in Hamilton in May.
The ICC program has been further enabled by St. Joseph’s Healthcare Hamilton’s implementation of Epic (Dovetale), which went live at St. Joseph’s in December 2017. At that time, said Coxon, St. Joe’s became a digital hospital and jumped to HIMSS EMRAM Stage 6. “Previous to that, we were at EMRAM 1.2,” she said. “It was an over-night transformation.”
The Epic implementation at St. Joseph’s Healthcare Hamilton was named Dovetale to signify the joining of technology with compassion. The system is helping to smooth out some of the pain points in Ontario’s healthcare system, specifically the hand-offs that occur when patients move from one level of care to another.
In one recent instance, a lung cancer patient who underwent surgery at St. Joseph’s was discharged home to Beamsville, only to discover that his wound seemed abnormal. He was worried it might have become infected.
He contacted his ICC coordinator at St. Joseph’s using the one-number service, and she instigated an ad hoc video visit to view the wound in real-time and determined that the patient should receive care right way.
This was arranged through St. Joseph’s Home Care, and on the same day, a visiting nurse travelled to the patient’s home and changed his wound dressings. She also updated his chart, right on the spot.
St. Joseph’s is making medical records available to the patients themselves through the use of a portal – called MyDovetale. “We were hearing that patients wanted better access to their records and that they wanted their records to be accurate and accessible throughout the system,” said Lukich.
In the summer of 2018, St. Joseph’s went live with the MyDovetale portal, extending it to patients in the mood disorder and kidney transplant clinics.
Patients can access their records on any platform, but it’s been found that smartphones are now the most popular device. Access can be given to family members, loved ones and members of care teams. Lukich said that 88 percent of patients report that MyDovetale has allowed them to take better care of themselves. Meanwhile, the video visit service has saved some patients two to three hours of travel time.
Patients have been asking for enhancements to the MyDovetale solution – in particular, they’d like to see prescription renewals and diagnostic imaging reports made available on the system.
MyDovetale will soon be rolled out to 80,000 more patients – an organization-wide rollout.
According to St. Joseph’s, the ICC program has resulted in a savings of up to $4,000 per patient, a 30 percent reduction in emergency department visits and 30 percent reduction in hospital readmissions with a 98 percent patient satisfaction approval rating. It’s doing this by enabling patients to stay comfortably in their homes, getting the reassurance or care they need without visiting the hospital.
The program has been so successful that Ontario’s health ministry would like to expand it to other healthcare providers.
“Already, St. Joseph’s has coached over 30 other organizations on how they might implement an ICC model of their own,” commented Fraser Edward, VP partnerships at SJHS.
“We have established the Centre for Integrated Care to help support Ontario Health Teams and other healthcare providers wrap physical and virtual care around the needs of patients and their families.” For more information, see: www.sjhs.ca/integratedcare/cic/






