How is the St. Joseph’s Health System’s Integrated Comprehensive Care program reducing hallway medicine?
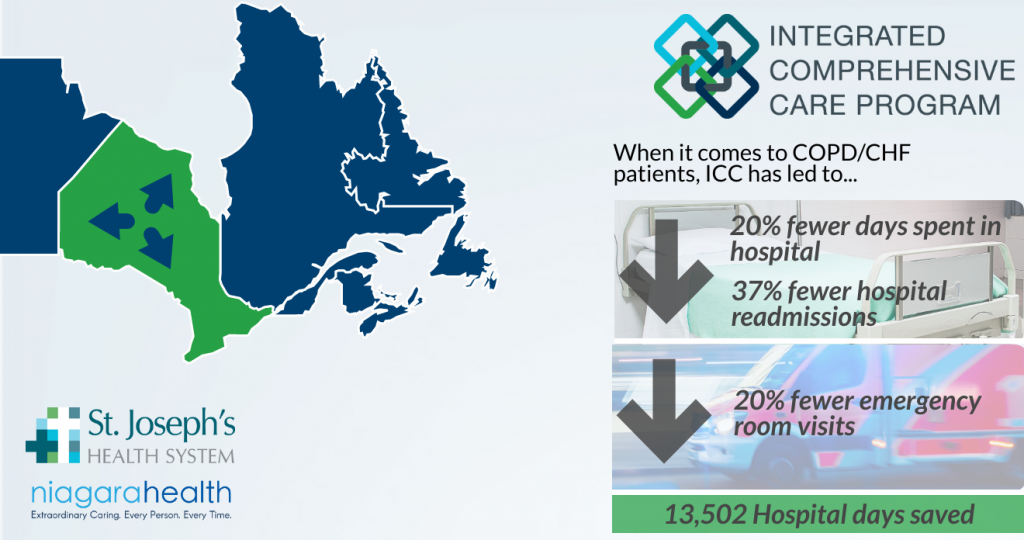
Jun 27, 2019St. Joseph’s Health System’s pioneering Integrated Comprehensive Care model for COPD/CHF patients could free up 13,502 hospital days annually across the province: Health System Performance Research Network (HSPRN)
June 27, 2019 – Hamilton, ON – A program pioneered by St. Joseph’s Healthcare Hamilton and St. Joseph’s Home Care, members of St. Joseph’s Health System (SJHS), has the potential to free up more than 13,000 hospitals days and save $24.1M in health care if it were spread across the province, according to a new research report.
Conducted by University of Toronto-affiliated Health System Performance Research Network (HSPRN) the evaluation analyzes six existing healthcare programs in Ontario with the aim of creating seamless transitions from hospital to home care. This is done by integrating care for patients through one team, one number to call 24/7 and one electronic record to support their care and save healthcare dollars – the key principles outlined in the government’s vision for Ontario Health Teams
St. Joseph’s Health System pioneered this model of care when it developed Integrated Comprehensive Care (ICC) in 2012. The MOHLTC later expanded the model to other sites throughout the Province, and SJHS partnered to expand ICC across 12 acute centres in the Hamilton Niagara Haldimand Brant (HNHB) Local Health Integration Network (LHIN) for all Chronic Obstructive Pulmonary Disease (COPD) and Congestive Heart Failure (CHF) patients. SJHS was also brought on board by the MOHLTC to support the provincial roll out. The HSPRN report evaluates this expansion.
The evaluation found that all six programs are having a positive effect on reducing hallway medicine. In particular, the total number of days patients spent in the hospital was reduced by more than 20%, readmissions were also reduced up to 37%, and there was an overall 20% relative reduction in Emergency Department visits. In addition, the report highlights that if the SJHS’ COPD/CHF ICC model was spread provincially to all 18,538 patients in Ontario, estimated annual savings of 13,502 hospital days and $24.1M dollars could be achieved.
“I was surprised at how successful HNHB ICC was at improving the transition of care for people with complex medical conditions,” says Walter Wodchis, Principal Investigator of the report and a Professor at the University of Toronto. “The collaboration they built between hospital and post-acute providers was crucial. I don’t think there has been another program that’s been quite [this] successful internationally.”
“This program was created by a group of nurses, PSW’s and frontline workers from the bottom up,” says Danielle Fox, St. Joseph’s Home Care Nurse. “We were given autonomy and flexibility to do what we needed to provide care to the patients. The one team approach and our focus around continuity of care, building rapport and educating caregivers/families as part of the care team are the keys to its success.”
The report recommends the MOHLTC implement a similar model of care for surgical procedures. Earlier this year, St. Joseph’s Healthcare Hamilton and Niagara Health announced they would be one of the first acute hospitals in Ontario to provide ICC program to all planned surgical patients with virtual care options by the end of 2019.
“The results speak for themselves,” says Dr. Thomas Stewart, President & CEO of St. Joseph’s Health System and CEO of Niagara Health. “We’re breaking down silos and working together with primary care and community partners. By coordinating our patient’s care from hospital to home, we not only see favourable outcomes for our patient’s and caregiver’s health, physically and mentally, but we are contributing to ending hallway medicine by freeing up much-needed beds and resources. It’s a win-win.”
ICC Patient/Caregiver testimonials:
• “It’s a marvellous thing. If there’s any chance that I can continue the program, I would jump at the chance. This team is the best, and I have never had anything like it.”
• “It was excellent. All the people that were involved were great. I wish that I’d known about it sooner.”
• “The ICC program has been an excellent help for me and my husband. It was comforting to know there was someone I could call for answers to any health concerns that might arise. The nurses, physiotherapist and dietitian, were all most pleasant and provided much valuable information to best help my husband, and therefore, me!!”
Quick Facts:
• St. Joseph’s Health System pioneered Integrated Comprehensive Care (ICC) and was the first healthcare initiative in Ontario to show the benefits of an Integrated Care approach between the hospital and the community. To learn more about the ICC Program: https://sjhs.ca/integratedcare/
• St. Joseph’s Home Care is the lead Home Care Agency for the HNHB ICC program. Nurses, PSW’s, Physiotherapists and other frontline staff are educated on caring for specific patient streams within the ICC program. To learn more about St. Joseph’s Home Care: https://www.stjosephshomecare.ca/
• Niagara Health, serving over 450,000 residents, contributes to the highest proportion of patients in the COPD/CHF program across HNHB. To learn more about Niagara Health: https://www.niagarahealth.on.ca/
Project partners:
HNHB Community Care Access Centre, HNHB Local Health Integration Network, HNHB Primary Care lead, Brant Community Healthcare System, Centre de Santé Communautaire, Grand River Community Health Centre, Haldimand War Memorial Hospital, Hamilton Health Sciences, Joseph Brant Hospital, Niagara Falls Community Health Centre, Niagara Health, Norfolk General Hospital, North Hamilton Community Health Centre, ProResp, SE Health, St. Joseph’s Healthcare Hamilton, St. Joseph’s Home Care, VitalAire, West Haldimand General Hospital
About St. Joseph’s Health System
St. Joseph’s Health System is one of the largest healthcare organizations in Canada, and only system in Ontario delivering a full continuum of health care services. Medical and specialty services affect care at all points and include acute care, long-term care, home care, hospice and research & education. SJHS is a globally recognized leader for innovation in models of patient-centred integrated care. St. Joseph’s Health System has a unique partnership with Niagara Health to leverage each organization’s strengths to bring better care to the people in the communities we serve.
About Niagara Health
Niagara Health (NH) is a community-based academic centre with a focus on teaching and learning, research and innovation. We are very proud of our strong partnership with the St. Joseph’s Health System and our academic partners including McMaster University, Brock University and Niagara College. Serving more than 450,000 residents across 12 municipalities making up the Regional Municipality of Niagara, NH is a regional healthcare provider with multiple sites and a growing network of community-based services. The team is made up of more than 4,800 employees, 600 physicians, and 850 volunteers to deliver ‘Extraordinary Caring. Every Person. Every Time’. We provide a wide range of inpatient and outpatient services to residents across Niagara, including Acute Care, Cancer Care, Cardiac Care, Complex Care, Emergency and Urgent Care, Kidney Care, Mental Health and Addictions, Stroke Care, Surgical Care and Long-Term Care.

